Hilda Hernández Álvarez
Cesar Bedoya Pilozo
Misladys Rodríguez
Lázara Rojas Rivero
Letter to the editor
Achatina fulica infected by Angiotrongylus cantonensis in Napo, Ecuador
Luis Solórzano Álava ![]() 1, Clinical pathologist
1, Clinical pathologist
Hilda Hernández Álvarez ![]() 2, Biochemist, Doctor of Science
2, Biochemist, Doctor of Science
Cesar Bedoya Pilozo ![]() 1, Aquaculturist, Master's degree in Molecular Biology
1, Aquaculturist, Master's degree in Molecular Biology
Misladys Rodríguez ![]() 2, Public Health Physician
2, Public Health Physician
Lázara Rojas Rivero ![]() 2, Microbiologist Physician, Doctor in Medical Sciences
2, Microbiologist Physician, Doctor in Medical Sciences
1 Instituto Nacional de Investigación en Salud Pública (INSPI), Guayaquil, Ecuador.
2 Instituto Pedro Kouri, La Habana, Cuba.
To the editor. Angiostrongylus cantonensis is a zoonotic parasite recognized as one of the main pathogens associated with meningitis and/or eosinophilic meningoencephalitis (1). In 2008, the first outbreak of natural transmission of A. cantonensis was described in Ecuador. It is currently a neglected parasitosis with evident underreporting of cases (2), even though it is one of the four zoonotic events notifiable to the Ministry of Public Health (MSP). In 2019, the surveillance system (SIVE-ALERT) of the MSP reported 85 cases of leptospirosis, 27 of brucellosis, and no cases of rabies and plague during the previous ten years. As for eosinophilic meningitis, the last case was officially reported in 2017 (3).
The life cycle of this parasite requires definitive and intermediate hosts. It is known that rats are the definitive hosts of A. cantonensis, after ingestion of the L3 larvae, which migrate to the central nervous system (CNS) where they mature into L4 and L5 larvae, developing into adult worms. When they reach sexual maturity, they lay their eggs in the pulmonary arteries; these develop into L1 larvae that migrate to the trachea where they are swallowed, passing into the gastrointestinal tract and excreted in the feces. Feces with larvae are ingested by snails that act as intermediate hosts, and progress to the L3 larval stage (infective larva for the definitive and accidental host). Humans are not the definitive host of the parasite, but become an accidental host by ingesting intermediate hosts or carriers containing infected larvae. In humans, the parasite does not complete its life cycle, but remains in the CNS, causing eosinophilic meningitis, or may settle in the eye chamber, causing ocular angiostrongyliasis (4).
In previous studies on snails in several regions of the country, the province of Napo shows high infection rates of 30.0% (unpublished data from the Instituto de Investigación en Salud Pública [INSPI]) and 27.16% (2). Therefore, the aim of this research, which included a larger number of intermediate hosts and a larger geographical extension, was to establish the infection rate and the average intensity of infection by A. cantonensis in the Achatina fulica snail in three cantons of the Napo province (Archidona, Tena and Arosemena Tola).
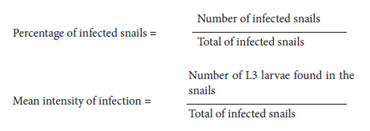
Between June and September 2019, specimens of the A. fulica snail were collected in the Napo province, which has an area of 13,271 km2, an altitude of 500 MSL, rainfall of 5000 mm per year, a temperature of 25 °C and humidity of 90 to 100%. The manual capture of these intermediate hosts was carried out using the method of capture per unit effort in 15 min (2). The snails were transported to the INSPI Laboratory, where they were examined for the presence of L3 larvae of A. cantonensis using the Lobato Paraense method for the extraction of soft organs (5). The paleal membrane was separated and placed in digestion solution for 6 hrs (6). L3 larvae were identified using a Motic SMZ-168 ™ stereomicroscope and an Olympus CX31 TM microscope. The percentage of infection and the average intensity of infection by A. cantonensis in intermediate hosts were determined as follows:
A total of 1476 specimens were collected, the percentage of snails infected with A. cantonensis was 46.5% (687/1476). The number of larvae found in the 687 infected A. fulica was 2236, i.e., the average intensity of infection was 3.3 L3 larvae per infected snail (Table 1).
Table 1. Percentage of intermediate hosts infected with A. cantonensis in three cantons of Napo (Tena, Carlos Julio Arosemena, Archidona) Ecuador.
|
Studied Cantons |
Location |
Number of collected specimens |
Number of infected snails |
Percentage of infection in the snails |
Number of L3 larvae |
Mean intensity of the infection |
|
Archidona |
Archidona |
100 |
54 |
54.0 |
272 |
5.0 |
|
Tena |
Ahuano |
120 |
59 |
49.2 |
212 |
3.6 |
|
Pano |
100 |
30 |
30.0 |
90 |
3.0 |
|
|
Puerto Napo |
100 |
66 |
66.0 |
125 |
1.9 |
|
|
Misahuallí |
100 |
60 |
60.0 |
168 |
2.8 |
|
|
Talag |
135 |
24 |
17.8 |
110 |
4.6 |
|
|
Casa del Diabético |
100 |
45 |
45.0 |
60 |
1.3 |
|
|
Paushiyacu |
100 |
42 |
42.0 |
197 |
4.7 |
|
|
Urbano Tena |
100 |
23 |
23.0 |
70 |
3.0 |
|
|
Satelital Tena |
100 |
61 |
61.0 |
183 |
3.0 |
|
|
Muyuna |
100 |
55 |
55.0 |
176 |
3.2 |
|
|
Surroundings of the Hospital José M. Velas co Ibarra |
100 |
54 |
54.0 |
80 |
1.5 |
|
|
Shandia |
121 |
44 |
36.4 |
150 |
3.4 |
|
|
Total Arosemena |
Total Arosemena |
100 |
70 |
70.0 |
70.0 |
4.9 |
|
|
Total |
1476 |
687 |
46.5 |
2236 |
3.3 |
L3: Infective larva for the definitive and accidental host
The study included only the species A. fulica because it is the most prolific intermediate host species, has the highest number of viable eggs, is terrestrial and was found in greater numbers in the studied locations, unlike other intermediate host species that are found in freshwater.
The results reveal a wide distribution of A. fulica infected with A. cantonensis and a higher percentage of infection than what has being reported by previous studies. These results have implications for the zoonotic transmission of the parasite, as human infection is mediated by infected intermediate hosts; ingestion is the main route of transmission, and shows that a considerable number of people are at risk of being infected, either through existing culinary traditions or through contamination of food with the infecting larvae. Strategies to minimize human infection should include community-targeted educational interventions, snail control to reduce the likelihood of ingestion, proper cooking of intermediate hosts, and education on the preparation of food to prevent the occurrence of sporadic cases and outbreaks of the disease.
Author contributions: Article conception: LSA, HHA, LRR, MR; data collection: LSA; analysis and interpretation; LSA, HHA, LRR; writing of the final version: LSA, LRR, HHA, CBP.
Conflicts of interest: Participants reported no conflicts of interest.
Funding: Self-funded.
REFERENCES
1. Martins YC, Tanowitz HB, Kazacos KR. Central nervous system manifestations of Angiostrongylus cantonensis infection. Acta Trop. 2015;141(Pt A):46-53. doi: 10.1016/j.actatropica.2014.10.002.
2. Solórzano L, Sánchez-Amador F, Valverde T. Angiostrongylus (Parastrongylus) cantonensis on intermediate and definitive hosts in Ecuador, 2014- 2017. Biomedica. 2019;39(2):370-84. doi: 10.7705/biomedica.v39i3.4387.
3. Ministerio de Salud Pública. Subsistema de vigilancia SIVE-ALERTA enfermedades zoonóticas Ecuador, SE 1-49 [Internet]. [cited on January 25, 2022]. Available at: https://www.salud.gob.ec/wp-content/uploads/2020/01/ZOONOTICAS-SE-49.pdf.
4. Wang Q-P, Wu Z-D, Wei J, Owen RL, Lun Z-R. Human Angiostrongylus cantonensis: an update. Eur J Clin Microbiol Infect Dis. 2012;31(4):389- 95. doi: 10.1007/s10096-011-1328-5.
5. Paraense WL. Lymnaea Diaphana; a study of Topotypic specimens (Pulmonata: Lymnaeidae). Mem Inst Oswaldo Cruz. 1984;79(1):75-81.
6. Wallace GD, Rosen L. Studies on eosinophilic meningitis. IV. Experimental infection of fresh-water and marine fish with Angiostrongylus cantonensis. Am J Epidemiol. 1967;85(3):395-402. doi: 10.1093/ oxfordjournals.aje.a120701.
Cite as: Solórzano Álava L, Hernández Álvarez H, Bedoya Pilozo C, Rodríguez M, Rojas Rivero L. Achatina fulica infected by Angiotrongylus cantonensis in Napo, Ecuador. Rev Peru Med Exp Salud Publica. 2022;39(1):122-3. doi: https://doi.org/10.17843/rpmesp.2022.391.10148.
Correspondence: Luis Solórzano Álava; lsolorzano@inspi.gob.ec
Received: 19/11/2021
Approved: 23/02/2022
Online: 31/03/2022