Pierina P. Cubillas-Espinoza
Eli L. Malvaceda-Espinoza
Original article
Psychological coping in female breast cancer patients from a metropolitan lima hospital
Fiorella D. Rivera-Cruzatt ![]() 1, Bachelor’s Degree in Psychology
1, Bachelor’s Degree in Psychology
Pierina P. Cubillas-Espinoza ![]() 1, Bachelor’s Degree in Psychology
1, Bachelor’s Degree in Psychology
Eli L. Malvaceda-Espinoza ![]() 1, psychologist, Ph.D. in Psychology
1, psychologist, Ph.D. in Psychology
1 Universidad San Ignacio de Loyola, Lima, Peru.
The present study is part of the research: Rivera-Cruzatt Fiorella Denisse y Cubillas, Espinoza Pierina Pamela. Afrontamiento psicológico en pacientes mujeres con cáncer de mama en un hospital de Lima Metropolitana [research project for the academic degree of bachelor in Psychology]. Lima: Facultad de Humanidades, Universidad San Ignacio de Loyola; 2020. Disponible en: https://repositorio.usil.edu.pe/items/72bf86d5-56b0-4671-813d-c2431bd20b16
ABSTRACT
Objective. To understand the psychological coping strategies in female patients with breast cancer from a hospital in Metropolitan Lima. Materials and methods. This was a qualitative research with a reflexive thematic analysis design. Sixteen women with breast cancer between 35 and 65 years of age were interviewed. Data was analyzed with the ATLAS.ti 22 software. Results. Three psychological coping strategies were described: emotional coping, which was found more frequently, includes the support of important people, religious coping, and focusing on positive consequences, which leads to a positive reinterpretation and progressive acceptance of the disease; active coping, characterized by diligent action, following indications, and seeking professional support. Finally, avoidance coping, which focuses on negative elements, postponement of the coping process and cognitive and behavioral distractions, the latter being of utmost relevance to balance the activities in the patients’ daily lives. Conclusions. Participants used emotional coping strategies more frequently, since they tried to increase positive emotions, accompanied by religious and environmental support. In addition, they also used active coping strategies, since they focused their actions to receive medical attention and treatment, leaving aside other activities; in spite of this, they used strategies to take their focus off the condition and thus detach themselves from their worries.
Keywords: Coping Strategies; Patient; Women; Breast Neoplasms; Qualitative Research (Source: MeSH NLM).
INTRODUCTION
In 2020, breast cancer caused the death of approximately 685,000 women worldwide and was detected in about 2.2 million women (1). During that year, 6860 cases were diagnosed in Peru, of which 63% were between 35 and 64 years of age (2,3). Treatment for this condition is affected by the health status, eating disorders, consumption behavior and oral contraceptive methods (4). Thus, medical treatment can range from surgery to general removal of breast tissue, combined with chemotherapy, radiotherapy, pharmacological therapy, among others; these treatments can trigger side effects both in the reproductive and sexual aspect, such as the inability to have children, which creates greater concern in women (5,6).
Likewise, women face states of vulnerability, confusion, worry, hopelessness and uncertainty during while adapting to the diagnosis, (7-10). This causes low self-esteem (11), feelings of inferiority (7), emotions like anger, guilt, grief and fear (7,8,12,13), and can even trigger disorders such as depression and anxiety (7,14), as well as high levels of stress (7,9,10). These psychological effects increase in a pandemic context, since it is more difficult to obtain essential elements by maintaining social distancing, besides women prefer to maintain communication with online support groups because they perceive limited social support from friends and family (4,15).
Even when family support is provided, economic problems and communication failures can cause the separation of some family members, resulting in feelings of frustration and misunderstandings, even when support is positive, physical or emotional dependence can occur (12,13). Therefore, it is essential to understand the coping strategies that women use during and after learning of their diagnosis (7,14). In this sense, psychological coping is understood as the cognitive or behavioral tasks carried out by the person, in order to psychosocially adapt to a problem (16). Such coping is divided into strategies, based on a group of actions that vary according to the person’s environment and other factors (17).
In this regard, the emotional coping style (16,18) includes strategies (family and friend support, religious support, positive transformation, denial and acceptance) that allow adjusting the level of emotional suffering caused by such health condition (19). In addition, the resolute coping style (16,18), involves strategies (diligence, professional support, postponement of coping actions, planning, omission of ordinary activities), with the aim of reducing the stress, and promoting positive psychological and emotional attitudes (17,18,20). The avoidant coping style (18) includes strategies (concentration and manifestation of adverse effects, cognitive distraction and behavioral distraction), where the individual shows disinterest in the intimidating event (18,19) in order to avoid the problem.
Previous research shows that, globally, the most used coping strategies by women are related to conflict solving (17,20). In addition, variables such as age, sentimental status and schooling are taken into account when choosing a strategy (21). In Peru, the emotional coping style is the most used one and it involves religious coping and positive reinterpretation strategies (19,22); however, avoidant coping strategies are less frequent (22). In this regard, patients show that the more professional support they receive, the greater their psychological coping will be (7); likewise, this support can come from the healthcare personnel, by being warm and empathetic, encouraging healthy eating habits, hygiene and showing a positive emotional state (23).
These studies were conducted in Peru and followed a quantitative approach, so they did not collect in-depth information on the phenomenon; therefore, we aim to address this theoretical gap through empirical evidence using qualitative methodological tools. At the same time, this will help more women to identify and use positive coping strategies, besides showing the importance of the psychological support provided to them. Accordingly, this study aims to understand psychological coping of female patients with breast cancer in a hospital in Metropolitan Lima.
|
KEY MESSAGES |
|
Motivation for the study: it is important to identify the coping strategies used by women with breast cancer, in order to contribute to their physical and emotional well-being. Main findings: strategies related to the emotional sphere are used to a greater extent, and also lead to progressive acceptance of the disease. Cognitive and behavioral distractions are necessary to balance patients’ daily activities. Implications: understanding how women face this disease allows the development of primary care strategies to improve their wellbeing. |
MATERIALS AND METHODS
Type and design
This study followed a qualitative approach and had a reflexive thematic analysis design. The former allowed for in-depth analysis of the study subject in its natural environment, reviewing the data and determining its categories (24). The design of this research allows the understanding of the information by focusing on the topics determined by the participants and explained by the researchers, associating the data according to patterns in relevant topics (25).
Participants
We included sixteen women aged 35 to 65 years (Table 1) diagnosed with breast cancer who received medical care at a level-3 public hospital in Metropolitan Lima, which specializes in oncological care. We applied convenience sampling, which is used when there is little accessibility to the population (26); this is the case of the present study, where the subject matter is associated with severe disease.
Table 1. Characteristics of the participants.
|
Pseudonym |
Age |
Employment |
Marital status |
Family composition |
Stage at diagnosis |
Age at diagnosis |
|
AA |
64 |
Nurse |
Married |
Husband and son |
II |
63 |
|
OS |
46 |
RH |
Married |
Husband and sons |
II |
44 |
|
DA |
59 |
RH |
Married |
Husband and son |
III |
54 |
|
DN |
52 |
Nursing Technician |
Married |
Husband and sons |
II |
51 |
|
JI |
59 |
Independent |
Married |
Children and niece |
II |
58 |
|
TC |
56 |
Administrator |
Married |
Husband and sons |
II |
55 |
|
MR |
48 |
Teacher |
Married |
Husband and sons |
II |
47 |
|
AR |
65 |
RH |
Single |
Sister and niece |
III |
60 |
|
SU |
51 |
Independent |
Single |
Mother and siblings |
III |
49 |
|
YJ |
59 |
RH |
Married |
Husband and sons |
III |
56 |
|
LG |
64 |
Independent |
Married |
Husband |
III |
63 |
|
TH |
59 |
RH |
Married |
Husband and daughters |
III |
58 |
|
SF |
51 |
Cosmetologist |
Married |
Husband |
II |
48 |
|
RS |
48 |
Independiente |
Married |
Son, parents and siblings |
III |
43 |
|
SN |
35 |
Accountant |
Single |
Father |
III |
31 |
|
CR |
51 |
RH |
Married |
Husband and sons |
II |
46 |
RH: responsible for the household, II: stage 2 breast cancer, III: stage 3 breast cancer.
Patients in stages II and III were included, detected at least one year before this research. Those who presented physical comorbidity or some psychopathological alterations were excluded, due to the differences in terms of treatment, physical and psychological consequences, process of adaptation to the diagnosis, professional and family support, as well as in the care provided by the hospitals that specialize in cancer (5,13).
Instruments for data collection
We used a semi-structured interview (Table 2) that was constructed based on the theoretical contributions about psychological coping explained from the topics of emotional, resolute and avoidant coping (18). The interview guide was evaluated by ten expert judges, health professionals knowledgeable about cancer patients, who evaluated the clarity, coherence and representativeness of the questions; their approval was obtained in order to carry out the interviews. A pilot interview was conducted by telephone call, which helped refine the questions for the final interview guide.
Table 2. Guiding questions.
|
Topics |
Guiding questions |
|
Emotional coping |
Who did you turn to for emotional support during your illness?
|
|
Resolute coping |
At what point did you begin to take action to address the illness?
|
|
Avoidant coping |
What aspects of your illness do you consider that you focus on? How
do you express the emotions derived from these consequences? |
Source: own elaboration.
Procedures
First, we reached out to the president of a group of breast cancer patients from a hospital in Lima via a social network; with her approval, the patients were contacted for the first time. We contacted 37 women, 17 of whom agreed to participate in the research; however, only 16 met the inclusion criteria. Subsequently, the participants were informed about the purpose of the research. They gave their informed consent orally, which was recorded on audio files. Likewise, they were told about the confidentiality, anonymity (use of pseudonyms), beneficence and nonmaleficence principles that guided this research.
Subsequently, the interviews were scheduled and then conducted via telephone calls. During the telephone calls, we ensured that the participants were alone and in a comfortable space (usually the living room of their home). The interviews were conducted between September and October 2020, and lasted an average of 40 minutes. The interviews, as well as the verbatim transcription, were carried out by the researchers FR and PC, who worked on an equal number of interviews. No patient refused to participate or dropped out of the study. Likewise, no payment was given for participating in the interviews, which were conducted in one session (there were no repetitions) and in Spanish.
Data analysis
We followed the guidelines of reflexive thematic analysis with a hybrid method (25). The process started with the familiarization with the data, through transcriptions. Subsequently, initial codes were generated and assigned to the relevant quotations in the document; at this point, a double cycle of coding by patterns, axial and selective, was carried out (27). In parallel, we generated, reviewed, and defined the themes, which were identified by the constant comparative method, grouping the codes into categories. Finally, we prepared the results report, where the strategies of meaning generation were found (28), such as the identification of patterns, which allows evidencing the saturation of the codes and/or categories; the count, which allows showing the magnitude of the codes throughout the analysis; and the density, which evidences the explanatory power of the codes, through their connections with other codes and/or categories. The categories that fulfilled at least one of the aforementioned tactics were considered as major themes. The analysis was carried out mainly by FR and PC, and they discussed and solved the discrepancies in the coding together with MS. The analysis was carried out with the support of ATLAS.ti 22 software.
Ethical and quality criteria
Permission was obtained from the ethics committee of the Graduate School of the Universidad Peruana Unión (No. 2022-CE-EPG-0000116). This article is adapted to the criteria of the Consolidated Criteria for Reporting Qualitative Research (COREQ) (29).
The present study meets quality criteria such as credibility (30), since the transcripts and results of the study were given to the participants to verify the information and obtain their opinions; however, there were no additional comments from them. It also complies with the confirmability criterion (30), since data collection, analysis and results can be traced and verified to their origin, which generates a logical chain of evidence. Next, auditability (31), which implied the triangulation of researchers by auditing the interview guide through 10 expert judges.
RESULTS
The 16 participants interviewed had an average age of 54 years. Stage II and III patients were distributed equally. Regarding their activities, six indicated that they were responsible for the household, while the other 10 had a trade or profession. Most of the women were married and their family structure consisted of a spouse and children or one of them. The ages at which they were diagnosed ranged from 31 to 63 years.
According to the analysis, breast cancer causes different psychosocial consequences, including dependence, physical weakness, as well as feelings of sadness, depression and frustration.
There I was, with more pain in my body, my bones hurt, I could no longer walk as much and I was in a wheelchair. SN, 35 years old.
In spite of this, the women showed a desire to continue treatment. This leads the participants to cope psychologically with their illness through different strategies such as emotional, resolutive and avoidant coping, which will be discussed below (Figure 1).
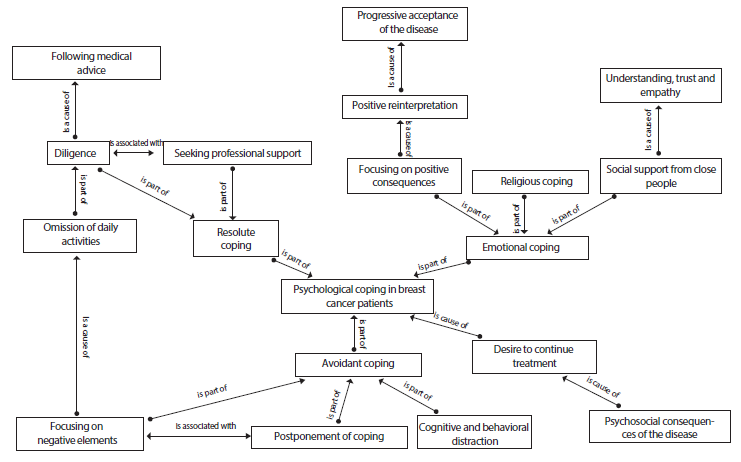
Figure 1. Semantic map of coping strategies in female breast cancer patients.
Emotional coping
This coping strategy was the most frequently found and involves actions focused on emotions, with the aim of improving the current situation. In this regard, the patients sought social support from close people, whether from family, friends, support groups or religious groups, this was important for stage III patients.
In my case, my friends at work told me: cheer up, SN, seek another opinion. SN, 35 years old.
This is a direct way of coping, with the aim of seeking understanding, trust and empathy. They also showed religious coping, which helped them become closer and strengthened their beliefs.
I am a believer, that was my support [...] I believed that God’s will was being clear with the relapses and I had to accept it [...] I am moving forward for my healing. CR, 51 years old.
On the other hand, participants also showed that they focus on the positive consequences of the disease, which leads them to generate a positive reinterpretation, as they recognize beneficial experiences in the face of what they have lived; at this point, they point out to carry out new activities and revalue daily activities (spending time with the family and improving self-care).
But as a result of this diagnosis, I have decided to do things that I was always thought of doing later. So, now I have dedicated myself to music, I plan to teach, it fills my soul, my life and everything. It's something I enjoy. TC, 56 years old.
An element that emerges from the positive reinterpretation is the progressive acceptance of the disease, thus, although they had feelings of fear and worry at the beginning, they later experienced surprise and tranquility, and came to accept the disease.
One has to live with it, there is nothing else to do, although you still miss your life before, the things you used to do. JN, 58 years old.
In this sense, women sought support from close personal environment, in search of understanding, trust and empathy, which made them feel accompanied in order to control the emotions caused by the disease.
Likewise, approaching religion made them feel that the disease is an obstacle to overcome, which gave them faith and strength, making them feel comforted while they focused on the positive consequences, either to avoid increasing negative emotions or because they had a more optimistic perspective of life situations in accordance with their personality, so they could have a positive reinterpretation, achieving a progressive acceptance of the disease.
Resolute coping
The patients, during their first experiences with the diagnosis, took diligent actions to intervene directly in the face of suspicions about their condition, especially when seeking a medical opinion to confirm their diagnosis and learn about the possible treatments they would have to undergo. In the face of this, they focused on following medical indications.
Just following what the doctors told me, right? They are the ones who tell you, first the surgery, the mastectomy, radiation, biopsy, an appointment for this, for that, they are the ones you have to follow. SF, 51 years old.
Therefore, the patients sought professional support, both physical and psychological, in order to reduce the adverse effects of the disease, which is representative of women in stage II.
When I went to the psychologist, he helped me a lot because I felt that this person made me feel calmer, I felt the hugs from the doctor who supported me, he always tells me: You are getting over it, you are doing fine. DN, 52 years old.
On the other hand, participants stated that they omitted daily activities, whether work, academic or home activities that they carried out before learning of their diagnosis, in order to focus all their temporal, mental and physical efforts to carry out the treatment and its implications.
Before, everything was normal, but when I found out, since then, I have been almost a year without working, since the treatment, the operations, the chemotherapy and now the radiotherapy take too much time [...] so, it is practically dedicating all that time to just cure yourself. TC, 56 years old.
Thus, the suspicion of breast cancer produces uncertainty, so in order to reduce it, patients seek medical attention to learn about their condition. When they already know about it, they focus on complying with medical indications, due to hasty decision making to avoid aggravation of their health. Thus, they seek professional support to improve their physical and mental condition; likewise, they are committed to set aside routine activities, studies and work, due to lack of time, motivation and physical limitations.
Avoidant coping
Some participants focused on the negative elements of their diagnosis (limitations regarding work, physical, emotional aspects, etc.), which made it difficult for them to continue with their daily activities. Therefore, they avoided these tasks, which caused them to postpone coping at a certain point, which implied an immobilizing reflection on the fact, hiding the diagnosis from those close to them and seeking different medical opinions before starting any treatment.
Well, to get closer, to verify, to have other opinions, until I rectified that, if it really was cancer, and to start with the treatment, right? TC, 56 years old.
Participants also reported focusing on other thoughts and activities in order not to focus on the disease, thus seeking cognitive and behavioral distraction, including family activities, helping others and having behaviors related to the improvement of their health. It is relevant to point out that although these distractors reorganize the patients’ activities, they are also necessary to balance their daily tasks. This was more significant in stage III patients.
Yes, to avoid thinking about my illness, I look for more things to do, if I finish cooking, washing the dishes, sewing, I give myself more work to do. It helps me to clear my mind and not have negative thoughts. MR, 48 years old.
In general, women who use avoidant coping are indifferent to the condition, so that, when they consider the negative elements, they prefer to postpone coping, either by avoiding prioritizing the diagnosis or by increasing the time dedicated to other activities in order to reduce the stress they are experiencing. In this way, thoughts related to worsening physical and emotional health will decrease.
DISCUSSION
The psychological coping of the patients is presented by means of emotional, resolutive and avoidant coping strategies. This is in agreement with the theoretical approaches previously mentioned (18). However, in contrast to previous studies (17,20), which reported that resolute coping was the most used, our results showed that the emotional coping strategy was the most frequently used (19,22). This may be due to the pandemic context, in which people required greater social support from close relationships. Patients with chronic diseases were at greater risk of Covid-19, this produced intense fear, together with sleep problems, anxiety, and particularly the need for psychological help, which would facilitate communication with family and friends and allow them to watch over their own mental health (32).
Continuing with emotional coping, the need to feel trust and empathy, as well as being understood by people close to them, is evident (18,33). On the other hand, regarding religious coping, the patients strengthened their beliefs, which decreased the tension caused by the condition; this may be due to the fact that religion promotes feelings of faith, hope and strength, thus diminishing the perception of the diagnosis as a threat (18,19,22).
Next, in terms of focusing on positive consequences, participants engaged in new entertainment activities, which favors coping (22). This produced a positive reinterpretation of the situation, which contributed to a positive acceptance of the disease (7,18,19,22). This acceptance may be due to the fact that the more women are aware of their diagnosis, the more opportunities they will have to regain control of their lives (19). Therefore, it can be argued that women revalue their family, personal and religious life, which allows them to continue with their daily activities (19,22).
Regarding resolution coping, participants acted diligently in the face of their condition, which increases behaviors related to following medical indications, as well as positive emotions about their diagnosis (17,18,20). Participants followed the guidelines provided by the medical staff in a meticulous manner, improving their perception of control and decreasing the impression of threat (17,19,20).
Likewise, women seek professional help to cope with their condition, which agrees with previous research (23), this is due to the intervention methods used by the professionals to promote the balance of emotions (33,34). It should be noted that professional support is fundamental, therefore if it decreases, coping would be at risk (23,33). Along the same lines, women omit daily activities related to different aspects of their lives when carrying out actions to mitigate the situation (22).
On the other hand, regarding avoidant coping, participants initially focused on the negative elements of their illness, leading to emotions of distress that are expressed through crying, which, if not sustained over prolonged periods of time, can contribute to adaptation (18). Likewise, they postponed their coping strategies in order to adapt to their disease, therefore, they did not take into account the development of an additional plan due to the short time elapsed since the knowledge of their diagnosis (18,19).
Furthermore, participants, mainly those in stage III, resorted to cognitive and behavioral distraction. In this sense, they carry out other activities, avoiding focusing on their diagnosis (18,34). Thus, patients seek balance between following medical advice and engaging in distracting activities (7).
One of the limitations of this study is that the interviews were conducted via telephone calls, which prevented the collection of nonverbal information. Other limitations include issues with the telephone signal, as well as not being able to ensure that the patient was in a suitable space to talk about sensitive issues, which could have affected the participant’s performance. The implications are based on understanding how psychological coping is employed by the women to deal with illness.
In conclusion, when faced with the psychosocial consequences of breast cancer, women employed different strategies. The emotional coping strategy stands out, in which they tried to increase positive emotions, either with the support of people close to them, religious support or by focusing on the positive consequences of the disease, as they all provide feelings of accompaniment, understanding, strength and tranquility. However, these strategies are also related to the personality of the patient, who, by having a more optimistic posture, try to face the condition similarly, avoiding focusing on the consequences and negative emotions. They also used problem-solving strategies, which helped them channel their efforts into taking action in the face of the disease, especially regarding medical care and treatment, therefore, they left aside other activities, postponing or skipping them in order to concentrate all their effort on physical and emotional recovery. On the other hand, women also used strategies to take their minds off the disease, as they focused on other activities, even initiating new projects that emerged as a way to detach themselves from their current concerns about their overall health.
Finally, we recommend that health professionals, family and friends should encourage an empathetic attitude towards the patient, since their actions influence the psychological coping process, favoring or harming the emotional health of women with breast cancer. Also, we suggest to further explore topics such as structured planning with self-initiative and ideas of abandonment of treatment, which turned out to be minor issues in this research, as they were found in a minimum number of cases.
Acknowledgments: to all those women who took the time to share their experiences with us.
Author contributions: FRC and PCE conceptualized, designed the methodology, conducted the research, analyzed the data, wrote the initial draft, and wrote and reviewed the final version. EME supervised and validated the methodology, data analysis, initial draft, and reviewed and approved the final version. EME provided the research resources and managed the research activities. FRC, PCE and EME assume responsibility for the article.
Funding: the research was self-funded.
Conflicts of interest: all authors indicate that they have no conflicts of interest.
REFERENCES
1. World Health Organization [Internet]. Breast cancer; 2021 [Citado 10 de Dic 2022]. Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/breast-cancer .
2. World Health Organization: International Agency for Research on Cancer [Internet].Estimated number of new cases in 2020, breast, female, all ages; 2021 [cited 2022 Dec 10]. Available from: https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=population&mode_population=countries&population=900&populations=900&key=asr&sex=2&cancer=20&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=0&ages_group%5B5D=17&group_cancer=0&include_nmsc=0&include_nmsc_other=1.
3. World Health Organization: International Agency for Research on Cancer [Internet]. Estimated number of new cases in 2020, breast, female, ages 35-64; 2021 [cited 2022 Dec 10]. Available from: https://gco.iarc.fr/today/online-analysis-table?v=2020&mode=population&mode_population=countries&population=900&populations=900&key=asr&sex=2&cancer=20&type=0&statistic=5&prevalence=0&population_group=0&ages_group%5B%5D=7&ages_group%5B%5D=12&group_cancer.
4. Dinapoli L, Colloca G, Di Capua B, Valentini V. Psychological Aspects to Consider in Breast Cancer Diagnosis and Treatment. Curr Oncol Rep. 2021;23(3):38. doi: 10.1007/s11912-021-01049-3.
5. Instituto Nacional del Cáncer [Internet]. Cómo se diagnostica el cáncer; 2019 [cited 2022 Dec 10]. Available from: https://www.cancer.gov/espanol/cancer/diagnostico-estadificacion/diagnostico .
6. Cancer.net: American American Society of Clinical Oncology [Internet]. Tomar decisiones respecto al tratamiento contra el cáncer; 2018 [cited 2022 Dec 10]. Available from: https://www.cancer.net/es/desplazarse-por-atención-del-cáncer/cómo-se-trata-el-cáncer/tomar-decisiones-respecto-del-tratamiento-contra-el-cáncer.
7. Gonzalez GC. Afrontamiento y apoyo social ante el diagnóstico reciente de cáncer de mama [bachelor thesis]. Lima: Facultad de Letras y Ciencias Humanas, Pontificia Universidad Católica del Perú; 2018. Available from: http://tesis.pucp.edu.pe/repositorio/bitstream/handle/20.500.12404/12242/Gonzalez_Castillo_Afrontamiento_apoyo_social1.pdf?sequence=1&isAllowed=y.
8. Correa M. Impacto psicológico frente al diagnóstico de cáncer de mama: primeras reacciones emocionales. Index Enferm. 2017; 26(4): 299-302.
9. Arrieta IR, Cárdenas JE, García MM, Gaviria A. Afrontamiento y calidad de vida en mujeres con cáncer de seno: revisión bibliográfica una mirada desde la psicología de la salud. Rev Univ Catol Luis Amigó. 2019; (3):115-26. doi: 10.21501/25907565.3261.
10. Ortiz N, Maldonado L. Cáncer de mama: Una mirada desde los procesos de afrontamiento psicológicos [undergraduate thesis]. Bogotá: Facultad de Ciencias Humanas, Universidad Cooperativa de Colombia; 2019. Available from: https://repository.ucc.edu.co/bitstream/20.500.12494/13745/1/2019_afrontamiento_cancer_mama.pdf .
11. Cerquera A, Matajira Y, García E, Vásquez E. Estrategias de afrontamiento en pacientes diagnosticados con cáncer de mama y el papel del psicólogo. Rev Psicol GEPU, 2017;8(2):144–54.
12. Jang M, Kim J. A structural model for stress, coping, and psychosocial adjustment: A multi-group analysis by stages of survivorship in Korean women with breast cancer. Eur J Oncol Nurs, 2018;(33):41–8. doi: 10.1016/j.ejon.2018.01.004.
13. Cancer.net: American Society of Clinical Oncology [Internet]. De qué manera el cáncer afecta la vida familiar; 2018. [cited 2022 Dec 10]. Available from: https://www.cancer.net/es/asimilacion-con-cancer/dialogo-sobre-el-cáncer/de-que-manera-el-cancer-afecta-la-vida-familiar.
14. Valderrama M, Sánchez R. Trastornos de ansiedad y depresión en relación con la calidad de vida de pacientes con cáncer de mama en estadio localmente avanzado o diseminado. Rev Colomb Psiquiatr. 2017;47(4):211–20. doi: 10.1016/j.rcp.2017.04.003.
15. Massicotte V, Ivers H, Savard J. COVID-19 Pandemic Stressors and Psychological Symptoms in Breast Cancer Patients. Curr Oncol. 2021;(28):294–300. doi: 10.3390/curroncol28010034.
16. Lazarus R, Folkman S. Estrés y procesos cognitivos. Barcelona, España; 1986.
17. Ruiz Doria SC, Valencia Jimenez NN, Ortega Montes JE. Condiciones de vida y estrategias de afrontamiento de las mujeres con cáncer de mama en Córdoba, Colombia. An Psicol [Internet]. 2020;36(1):46–55. doi: 10.6018/analesps.351701.
18. Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. J Pers Soc Psychol. 1989;56(2):267–83. doi: 10.1037/0022-3514.56.2.267.
19. Medina MP. Afrontamiento y optimismo disposicional en pacientes mujeres con cáncer de mama [bachelor thesis]. Lima: Facultad de Letras y Ciencias Humanas, Pontificia Universidad Católica del Perú; 2017. Available from: https://tesis.pucp.edu.pe/repositorio/bitstream/handle/20.500.12404/9108/MEDINA_OLANO_AFRONTAMIENTO_Y_OPTIMISMO_DISPOSICIONAL_EN_PACIENTES_MUJERES_CON_CANCER_DE_MAMA.pdf?sequence=1&isAllowed=y.
20. Moreno M, Gutiérrez D, García R. Afrontamiento al cáncer de mama en pacientes diagnosticadas. Enfermería Investiga [Internet]. 2017 [cited 2022 Dec 10];2(1):1–6. Available from: https://revistas.uta.edu.ec/erevista/index.php/enfi/article/view/756/784.
21. Acosta-Zapata E, López-Ramón C, Martínez-Cortés ME, Zapata-Vázquez R. Funcionalidad familiar y estrategias de afrontamiento en pacientes con cáncer de mama. Horiz Sanitario. 2017;16(2):139–48. doi: 10.19136/hs.v16i2.1629.
22. Lostaunau V, Torrejón C, Cassaretto M. Estrés, afrontamiento y calidad de vida relacionada a la salud en mujeres con cáncer de mama. Actual en Psicol. 2017;31(122):75. doi: 10.15517/ap.v31i122.25345.
23. Columbus CD. Apoyo emocional que brinda el profesional de enfermería y el afrontamiento de los pacientes con cáncer de mama de 30 a 50 años de la Unidad de Quimioterapia de la Clínica Oncosalud. [bachelor thesis]. Lima: Facultad de Medicina, Universidad Nacional Mayor de San Marcos; 2017. Available from: https://cybertesis.unmsm.edu.pe/bitstream/handle/20.500.12672/6970/Columbus_vc.pdf?sequence=3&isAllowed=y.
24. Creswell J, Poth CN. Qualitative inquiry and Research design: Choosing among five approaches (4th ed.). SAGE; 2018.
25. Braun V, Clarke V. Can I use TA? Should I use TA? Should I not use TA? Comparing reflexive thematic analysis and other pattern-based qualitative analytic approaches. Couns Psychother Res. 2021;21(1):37–47. doi: 10.1002/capr.12360.
26. Robinson OC. Sampling in Interview-Based Qualitative Research: A Theoretical and Practical Guide. Qual Res Psycho. 2014;11(1):25-41. doi: 10.1080/14780887.2013.801543.
27. Saldaña J. The Coding Manual for Qualitative Researchers. London: Sage Publications; 2013.
28. Miles MB, Huberman AM, Saldaña J. Qualitative Data Analysis. A Methods Sourcebook. Arizona State University: Sage Publications; 2013.
29. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349-357.
30. Mertens D. Research and Evaluation in Education and Psychology: Integrating Diversity with Quantitative, Qualitative, and Mixed Methods. Washington, United States: Sage Publications; 2015.
31. Ben Kei D. Empirical verification of the "TACT" framework for teaching rigour in qualitative research methodology. Qual Res J. 2018;18(3):262–75. doi: 10.1108/QRJ-D-17-00012.
32. Prieto-Rodríguez MA, March-Cerdá JC, Martín-Barato A, Escudero-Carretero M, López-Doblas M, Luque-Martín N. Repercusiones del confinamiento por COVID-19 en pacientes crónicos de Andalucía. Gac Sanit. 2022;36(2): 139-145. doi: 10.1016/j.gaceta.2020.11.001.
33. Mokhtari L, Markani AK, Khalkhali HR, Feizi A. The perceived social support by Iranian women with breast cancer: a qualitative study. Support Care Cancer. 2021;30(1):941–9. doi: 10.1007/s00520-021-06478-1.
34. Srivastava J, Kaushik S, Tewari M, Shukla H. Mediating role of affective experiences in the relationship between perceived social support and life satisfaction among breast cancer patients. Indian J Palliat Care. 2021;27(1):76–82. doi: 10.4103/IJPC.IJPC_106_20.
Cite as: Rivera-Cruzatt FD, Cubillas-Espinoza PP, Malvaceda-Espinoza EL. Psychological coping in female breast cancer patients from a Metropolitan Lima hospital. Rev Peru Med Exp Salud Publica. 2022;39(4). doi: https://doi.org/10.17844/rpmesp.2022.394.12322.
Correspondence: Eli L. Malvaceda-Espinoza; emalvaceda@usil.edu.pe
Received: 31/10/2022
Approved: 14/12/2022
Online: 22/12/2022