María del Carmen López-Talledo
César Galván-Calle
Ricardo Muñoz-León
Edgar Matos-Benavides
Crhistian Toribio-Dionicio
Wilmer Córdova-Calderón
BRIEF REPORT
Sensitization to aeroallergens
in a peruvian pediatric population with allergic diseases
David García-Gomero ![]() 1,2,
Medical doctor
1,2,
Medical doctor
María del Carmen López-Talledo ![]() 1,3, allergist-clinical immunologist
1,3, allergist-clinical immunologist
César Galván-Calle
![]() 1,3, allergist-clinical immunologist
1,3, allergist-clinical immunologist
Ricardo Muñoz-León ![]() 1,3, Pediatrician
1,3, Pediatrician
Edgar Matos-Benavides ![]() 1,3, allergist-clinical immunologist
1,3, allergist-clinical immunologist
Crhistian Toribio-Dionicio ![]() 1,2 ,
Medical doctor
1,2 ,
Medical doctor
Wilmer Córdova-Calderón ![]() 1,3, allergist-clinical immunologist
1,3, allergist-clinical immunologist
1
Centro de Referencia Nacional
d Alergia, Asma e Inmunología, Instituto Nacional de Salud del Niño, Lima,
Perú.
2 Facultad de Medicina,
Universidad Nacional Mayor de San Marcos, Lima, Perú.
3 Sociedad Peruana de
Inmunología, Lima, Perú.
ABSTRACT
In
order to determine the profile of sensitization to aeroallergens in pediatric
patients with asthma and / or allergic rh4initis, a cross-sectional study was
carried out in 411 patients using an allergy skin test. Age, sex, total IgE
level and eosinophils were analyzed. The mean age was 8.1 ± 3.7 years and 60.6%
were male. The average of the eosinophils and the level of total IgE was 450.1
± 377.3 cells / mm3 and 861.7 ± 757.6
IU / mL, respectively. Mites were the most frequent sensitizing allergens
(79.8%) and Dermatophagoides farinae (65.2%) was the most common.
Polysensitization was present in 76.2% of patients. Sensitization was evident
in the majority of patients with asthma and / or allergic rhinitis and was
associated with age, age groups and total IgE level.
Keywords: Allergic rhinitis; Asthma; Allergens; IgE-Mediated Hipersensitivity; Peru (source: MeSH NLM).
INTRODUCTION
Asthma
and allergic rhinitis (AR) are the most important chronic inflammatory diseases
in children, with a significant effect on the finances and life quality of
these patients (1-3). The prevalence of these diseases is increasing
worldwide, possibly due to factors, such as environment, diet or climate change (1).
Based on different studies conducted in Peru, asthma and AR have a prevalence
greater than 30% (4, 5), and they constitute the most frequent chronic
non-infectious diseases in patients of pediatric age.
Extra- or intradomiciliary aeroallergens are the main triggers of
allergic diseases (1). During the first two years, children are exposed to
intradomiciliary aeroallergens (dust mites, fungi, particles or animal
excretions), and since the age of five they are exposed to extradomiciliary
aeroallergens (pollen, fungi, grass) (1-3,6). Early exposure and the
presence of atopy in patients with asthma or AR contribute to the persistence
of these enzymes in adulthood (1-3). Sensitizing aeroallergens can vary
between countries; however, their identification is necessary for a better
clinical approach (1-3).
Atopy is the personal or familiar tendency to produce specific immunoglobulin E (IgE) antibodies in response to allergen sensitization (7). Its diagnosis is established by a compatible clinical history and is supported by skin testing (prick test) or in vitro tests that confirm sensitization or the presence of IgE against certain allergens (1-3). Skin testing is the most common test used to detect IgE-mediated reactions in patients with asthma and AR (1-3), because it has shown greater sensitivity and specificity (8) and has a lower rate of patient complications and discomfort (1-3).
|
KEY MESSAGES
|
|
Motivation for the study:
To
determine the sensitization profile of pediatric patients with asthma or
allergic rhinitis using a skin test, a fundamental step for an adequate and
specific management of allergic diseases.
Main findings:
Most patients with
asthma or allergic rhinitis present Dermatophagoides farinae sensitivity.
It is associated with age, age groups and IgE level.
Implications:
Our results should be considered complementary to the treatment of patients
with asthma or allergic rhinitis with specific immunotherapy based on their
sensitization. |
Because of
this, the identification of aeroallergens-sensitivity in patients with asthma
or AR is useful to implement preventive measures and to develope more effective
and targeted treatment strategies, such as allergen-specific immunotherapy, the
only type of therapy capable of modifying the abnormal immune response in
patients with allergic diseases, providing improvement in the symptomatology
and quality of life (1-3). The aim of this study is to establish the profile of
aeroallergen sensitization in Peruvian children with diagnosis of asthma or AR
due to the epidemiological significance and the need for specific interventions
in these patients.
THE STUDY
Cross-sectional
design. Patients were enrolled from January 2013 to December 2015 at the
National Reference Center for Allergy, Asthma and Clinical Immunology (CERNAAI)
of the National Institute of Children’s Health (INSN), a center specialized in
allergic and immunological diseases that receives patients from all over Peru.
The study population was of 411 patients who were selected
through a census sampling. We included patients from 2 to 17 years old, with
clinical diagnosis of asthma or AR, based on the GINA and ARIA criteria,
respectively (2,3). We excluded patients who had used antihistamines or
systemic corticosteroids, at least seven days before skin testing; topical
corticosteroids in the test area, at least 10 days before; patients in
immunotherapy, at least six months before; in immunoregulatory therapy (use of
intravenous immunoglobulin); with other immunological diseases (autoimmune or
lymphoproliferative diseases); with dermography and with hyper or hyporreactive
skin.
Data collected: age (categorized in groups: 2-5, 6-11 and 12-18
years old), gender, total IgE levels (IU/mL) and number of eosinophils in the
hemogram (cells/mm3). All patients were skin tested using the Prick-Film®
method to determine their specific allergens sensitivity. Results were obtained
in mm2 (papule area) and in mm (welt diameter). The
method used standard recommendations to indicate a positive result (9).
Sensitization was considered as a positive skin test result with
one aeroallergen and in the poly-sensitization with two or more aeroallergens.
The sensitization profile was classified by aeroallergen groups: dust mites,
insects, fungi and animal epithelium. Fourteen aeroallergens were applied (7
dust mites, 2 cockroaches, 3 fungi and dog and cat epithelium).
The data were analyzed with the SPSS program for Windows 20.0.
Percentages and frequencies were used for the description of qualitative
variables, and mean and standard deviation for quantitative variables. The
distribution of quantitative variables was analyzed using histograms, box plots
and the Kolmogorov-Smirnov test. The chi-square test was used to evaluate the
association between sensitization and age groups and gender. The Student T-test
was used for comparing means of the independent samples. Both tests used a 95%
confidence level.
Prior to
any procedure, parents or legal guardians voluntarily signed an informed
consent form. Patients over the age of seven were asked to sign an assent form.
The study protocol and the consent and assent forms were approved by the INSN
Institutional Research Ethics Committee and were in accordance with the principles
of the Helsinki Declaration (Project CL26-12).
RESULTS
The
average age of the population was 8.1 ± 3.8 years old. 60.6% were male, 83.5%
had asthma, 91.7% had rhinitis and 75.7% had AR. Among the patients with
asthma, 69.8% (287/343) had a positive skin test, and 83.7% (311/377) of
patients with AR had also a positive skin test. There is an increased frequency
of allergic phenotype (positive test) in patients with asthma and AR (Figure 1).
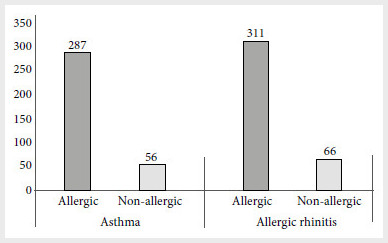
Figure 1. Allergic phenotype in 411 Peruvian pediatric
patients with asthma and allergic rhinitis
from the National Reference Center for Allergy, Asthma and Immunology, Lima.
The mean
for eosinophils was 450.1 ± 377.3 cells/mm3 and the total mean for IgE was
861.7 ± 757.6 IU/mL. As for the age groups, 32.4% were between 2 and 5 years
old, 47.9% between 6 and 11 years old and 19.7% between 12 and 18 years old
(Table 1).
Table 1. Characteristics of 411 Peruvian pediatric
patients with asthma or allergic rhinitis from the National Reference Center
for Allergy, Asthma and Immunology, Lima.
a Student T-test; b
Chi-square test
SD: Standard Deviation
Sensitization
profile
Sensitization
was present in 82.7% of the patients. Sensitization was associated with age,
age groups and total IgE levels (Table 1). The frequency of sensitization
increased with age (Table 2). The most frequent sensitizing agents were mites
(79.8%), followed by insects (42.3%) (Table 2). Only 6.6% of the patients were
sensitized by a single aeroallergen, while 47.7% of the patients were
sensitized by two to five aeroallergens, and 28.5% by six or more aeroallergens
(Table 3).
Table 2. Sensitization profile in 411 Peruvian
pediatric patients with asthma or allergic rhinitis from the National Reference
Center for Allergy, Asthma and Immunology. Lima.
The categories included in the table are not
mutually exclusive.
Table 3. Sensitization by number of allergens in 340
Peruvian pediatric patients with asthma or allergic rhinitis from the National
Reference Center for Allergy, Asthma and Immunology. Lima.
Dermatophagoides
farin
(DF) (65.2%), Dermatophagoides pteronyssinus (DP) (53%)
and Blomia tropicalis (47.7%) were the most frequent dust mites, 127
patients (30.9%) had a positive skin test for all three dust mites.
Sensitization to insects was mainly due to Blatella germanica (28.2%)
and Periplaneta americana (23.4%), while sensitization to fungi was
found in 17% of patients, Alternaria alternata being the most frequent
agent. Finally, sensitization to animal epithelia was found in 8.5% of
patients. Cat epithelium and dog epithelium were found in 6.8% and 3.4%,
respectively (Table 3).
DISCUSSION
Our study presents for the first time a sensitization profile
using a skin test in a Peruvian pediatric population with a diagnosis of asthma
or AR. It was shown that 82.7% of patients were sensitized by some aeroallergen
(76.2% to more than one) and was associated with age, age groups and total IgE
levels. Mites were the most frequent sensitizing agents, DF being the most
common (65.2%). The skin test was chosen for its higher sensitivity and
specificity (>85%) (7) and a lower rate of complications and patient
discomfort (1-3).
The skin test is recommended in clinical practice guidelines for asthma and AR
(GINA and ARIA, Respectively)
(2,3).
In Peru, some evaluations on sensitization profile have been
carried out. The study called PURA (Peru Urban versus Rural Asthma) whose
objective was to evaluate the prevalence of asthma and its associated risk
factors using the skin test in 13-15-year-old adolescents from two cities (one
urban and one rural) (10). The prevalence of asthma and the sensitization was
12% and 3%, and 56% and 38% in Lima and Tumbes, respectively. Further analysis
found that 61% of subjects with AR were sensitized (11). Sensitization was
lower compared to our study and could be due to the lower number of patients
with a diagnosis of asthma and AR. In Lima 84 patients had diagnosis of asthma,
and 166 had diagnosis of AR. On the other hand, in Tumbes 22 patients had
diagnosis of asthma and 95 had diagnosis of AR.
On the other hand, a case-control study conducted in two
communities in Lima included children between the ages of 9 and 19. From 412
asthmatic patients, 315 (78.2%) were atopic (12). These results are similar
to ours; however, it should be noted that the evaluation of atopy was performed
using ImmunoCap 250 (specific IgE serum detection) for three allergens (animal,
mold and dust mites) where a specific IgE level > 0.1 kU/L is a positive
result. This level may explain the high frequency of atopy, since a cut-off
point of > 0.35 kU/L is commonly used in other studies.
Different results exist in other contexts. The National Health
and Nutrition Examination Survey (NHANES) III, conducted in the United States
between 1988 and 1994, found a frequency of sensitization using a skin test in
54.3% of the 6-59-year-old study subjects (multiethnic population). (13). On
the other hand, a study in Morocco involving 379 patients found that 3.2% of
asthmatic patients were mono- and polysensitized, while 18.2% and 39.8% of
patients with AR were mono- and polysensitized, respectively (14). A
study performed in Spain showed sensitization to aeroallergens (measuring
specific IgE) in 25.9% (121/468) of patients between 0 and 5 years of age with
wheezing or atopic dermatitis (15). This difference in results could be
explained by the high prevalence of atopy and allergic diseases in our country,
as well as environmental factors such as climate, altitude and economic status.
DF was the most common aeroallergen; similar results have been
reported by other authors (13,15). However, some other authors
describe a greater sensitization to PD.
A study carried out in an urban area of Mexico found that this mite (DF)
was the most frequent allergen in school children with asthma (61%) (16),
as well as in Jordan (11.9%) (6) and in the United States (31.2%) (17),
the latter (US) being carried out on children with asthma who attended a
pediatric pulmonary center. On the other hand, the most frequent sensitizing
agents were olive pollen (18%) in Jordan (6). And in a study conducted in
Spain (18) the most frequent sensitizing agents were
grass (48%), tree (34%) and weed pollens (18%).
Other studies report insects in second or third place when
talking about frequency, reaching 21.6% (19), 26.1% (13) or 32% (17). The high sensitivity to
insects found in our study may be due to differences in housing and community
environments (13). In our study, Alternaria alternata was
predominant in fungal types. In contrast, Candida albicans and Cladosporum
were the predominant fungi in a Colombian study in 12.9% of the patients (20).
The frequency of sensitization was similar for cat and dog epithelium; similar
results are evident in other reports (13,14,16-19).
The limitations of our study comprise not considering the climate
where our patients reside, an aspect considered and recommended in other
studies that found a greater frequency of sensitization for pollens and other
allergens
(6,18), moreover, we used only the skin test to evaluate
sensitization and not the specific IgE level as other studies did (12,15,18).
In
conclusion, most patients with asthma or AR were sensitized based on skin test
results. The main sensitizing agent was DF, and sensitization was associated
with age, age groups and total IgE level.
Acknowledgements:
The authors are grateful to all the study participants, to the Executive Office of Support for Research and Specialized Teaching (OASIDE) and to the Institutional Committee on Research Ethics (CIEI) of the National Institute of Child Health (INSN).
REFERENCES
1. World Allergy Organization.
WAO White Book on Allergy: Update 2013 [Internet]. Milwaukee: WAO;2013 [citado
el 3 de diciembre de 2019]. Disponible en: https://www.worldallergy.org/wao-white-book-on-allergy.
2. Global Initiative for
Asthma. Global Strategy for Asthma Management and Prevention [Internet].
Fontana: GINA; 2019 [citado el 26 de noviembre de 2019]. Disponible en: https://ginasthma.org/2018-gina-report-global-strategy-for-asthma-management-and-prevention/.
3. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al.
Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration
with the World Health Organization, GA(2)LEN and AllerGen). Allergy.
2008;63 Suppl 86:8-160. doi: 10.1111/j.1398-9995.2007.01620.x.
4. Pearce N, Aït‐Khaled N, Beasley R, Mallol J, Keil U, Mitchell E, et al. Worldwide trends in the prevalence of asthma symptoms: phase III of the International Study of Asthma and Allergies in Childhood (ISAAC). Thorax. 2007;62(9):758-66. doi: 10.1136/thx.2006.070169.
5. Björkstén B, Clayton T, Ellwood P, Stewart A, Strachan D, ISAAC Phase III Study Group. Worldwide time trends
for symptoms of rhinitis and conjunctivitis: Phase III of the International
Study of Asthma and Allergies in Childhood. Pediatr Allergy Immunol. 2008;19(2):110-24. doi: 10.1111/j.1399-3038.2007.00601.x.
6. Al-Zayadneh EM, Alnawaiseh NA, Altarawneh AH, Aldmour IH, Albataineh EM, Al-Shagahin H, et al. Sensitization to
inhaled allergens in asthmatic children in southern Jordan: a cross-sectional
study. Multidiscip Respir Med. 2019;14:37. doi:
10.1186/s40248-019-0199-y.
7. Johansson SGO, Bieber T,
Dahl R, Friedmann PS, Lanier BQ, Lockey RF, et al. Revised nomenclature
for allergy for global use: Report of the Nomenclature Review Committee of the
World Allergy Organization, October 2003. J Allergy Clin Immunol.
2004;113(5):832-6. doi: 10.1016/j.jaci.2003.12.591.
8. Tschopp JM, Sistek D,
Schindler C, Leuenberger P, Perruchoud AP, Wüthrich B, et al. Current
allergic asthma and rhinitis: diagnostic efficiency of three commonly used
atopic markers (IgE, skin prick tests, and Phadiatop). Results from 8329
randomized adults from the SAPALDIA Study. Swiss Study on Air Pollution and
Lung Diseases in Adults. Allergy. 1998;53(6):608–13. doi: 10.1111/j.1398-9995.1998.tb03937.x.
9. Dreborg S, Backman A,
Basomba A, Bousquet J, Dieges P, Malling HJ. Skin tests used in type I allergy
testing Position paper. Sub-Committee on Skin Tests of the European Academy of
Allergology and Clinical Immunology. Allergy. 1989;44 Suppl 10:1-59.
10. Robinson CL, Baumann LM,
Gilman RH, Romero K, Combe JM, Cabrera L, et al. The Peru Urban versus
Rural Asthma (PURA) Study: methods and baseline quality control data from a
cross-sectional investigation into the prevalence, severity, genetics,
immunology and environmental factors affecting asthma in adolescence in Peru.
BMJ Open. 2012;2(1):e00421. doi: 10.1136/bmjopen-2011-000421.
11. Baumann LM, Romero KM, Robinson CL, Hansel NN, Gilman RH, Hamilton RG, et al.
Prevalence and risk factors for allergic rhinitis in two resource-limited
settings in Peru with disparate degrees of urbanization. Clin Exp Allergy. 2015;45(1):192-9. doi:
10.1111/cea.12379.
12. Nicholson A, Pollard SL,
Lima JJ, Romero K, Tarazona-Meza C, Malpartida-Guzmán G, et al. Serum
folate concentrations, asthma, atopy, and asthma control in Peruvian children.
Respir Med. 2017;133:29–35. doi: 10.1016/j.rmed.2017.10.026.
13. Arbes SJ Jr, Gergen PJ,
Elliott L, Zeldin DC. Prevalences of positive skin test responses to 10 common
allergens in the US population: results from the third National Health and
Nutrition Examination Survey. J Allergy Clin Immunol. 2005;116(2):377-83. doi:
10.1016/j.jaci.2005.05.017.
14. Bardei F, Bouziane H,
Kadiri M, Rkiek B, Tebay A, Saoud A. Skin sensitisation profiles to inhalant
allergens for patients in Tétouan city (North West of Morocco). Rev Pneumol Clin.
2016;72(4):221-7. doi: 10.1016/j.pneumo.2016.04.005.
15. Carvajal Urueña I, Díaz
Vázquez C, Cano Garcinuño A, García Merino A, Morell Bernabé JJ, Pascual Pérez
JM, et al. Perfil de sensibilización alérgica en niños de 0 a 5 años con
sibilancias o dermatitis atópica. An Pediatría. 2010;72(1):30–41. doi: 10.1016/j.anpedi.2009.09.011.
16. Alcalá-Padilla G,
Bedolla-Barajas M, Kestler-Gramajo A, Valdez-López F. Prevalencia de
sensbilización a alergenos en niños escolares con asma que viven en la zona
metropolitana de Guadalajara. Rev Alerg Mex. 2016;63(2):135–42. doi: 10.29262/ram.v63i2.184.
17. Nagarajan S, Ahmad S, Quinn M, Agrawal S, Manilich E, Concepcion E, et al. Allergic
sensitization and clinical outcomes in urban children with asthma, 2013-2016. Allergy
Asthma Proc. 2018;39(4):281-8. doi: 10.2500/aap.2018.39.4147.
18. Caro Rebollo J, Moneo
Hernández MI, Cabañas Bravo MJ, Garín Moreno AL, Oliván Otal MP, Cenarro
Guerrero T. Valoración del estudio alérgico en niños con atopia. Pediatría Aten
Primaria. 2010;12(46):227-37.
19. Sánchez-Borges M, Capriles-Hulett A, Torres J, Ansotegui-Zubeldia IJ, Castillo A, Dhersy A, et al. Diagnosis of allergic
sensitization in patients with allergic rhinitis and asthma in a tropical
environment. Rev Alerg Mex. 2019;66(1):44-54. doi:
10.29262/ram.v66i1.570.
20. Bissinger I, Bareño J.
Perfil de sensibilización a hongos en Medellín, Colombia. Rev Alerg Mex.
2016;63(2):123-34. doi: 10.29262/ram.v63i2.108.
Funding: Financial support was provided by the Executive Office of
Support for Research and Specialized Teaching (OASIDE) of the National
Institute of Child Health (INSN) (Project CL26-12).
Citation:
García-Gomero D, López-Talledo
MDC, Galván-Calle C, Muñoz-León R, Matos-Benavides E, Toribio-Dionicio C, et
al. Sensibilización a aeroalérgenos en una población pediátrica peruana con
enfermedades alérgicas. Rev Peru Med Exp Salud Publica.
2020;37(1):57-62. Doi:
https://doi.org/10.17843/rpmesp.2020.371.4460.
Keywords: Allergic rhinitis; Asthma; Allergens; IgE-Mediated Hipersensitivity;
Peru (source: MeSH NLM).
Correspondence to:
Wilmer
Córdova-Calderón; Centro de Referencia Nacional de Alergia, Asma e Inmunología,
Instituto Nacional de Salud del Niño; avenida Brasil 600. Lima, Perú;
wilmer.cordova@gmail.com
Authors’ contributions:
WCC, DGG, MCLT, CGC, RML and EMB contributed to the conception and design of
the work. DGG and CTD contributed to the data acquisition and analysis and
writing of the manuscript. WCC supervised the work. All authors contributed to
data interpretation, provided critical comments, and approved the final
version.
Conflicts of Interest:
All
authors have none to declare.
Received:
09/05/2019
Approved:
08/01/2020
Online:
23/03/2020