10.17843/rpmesp.2020.372.4772
ORIGINAL ARTICLE
Neonatal meningitis:
a multicenter study in Lima, Peru
Daniel Guillén-Pinto
 1,2, Pediatric neurologist
1,2, Pediatric neurologist
Bárbara Málaga-Espinoza
 1, physician
1, physician
Joselyn Ye-Tay  1, physician
1, physician
María Luz Rospigliosi-López
 1,2, neonatologist
1,2, neonatologist
Andrea Montenegro-Rivera
 1, pediatrician
1, pediatrician
María Rivas
 4, Pediatric neurologist
4, Pediatric neurologist
María Luisa Stiglich
 4, Pediatric neurologist
4, Pediatric neurologist
Sonia Villasante-Valera
 4, neonatologist
4, neonatologist
Olga Lizama-Olaya
 7, neonatologist
7, neonatologist
Alfredo Tori  7, Pediatric neurologist
7, Pediatric neurologist
Lizet Cuba
 5, physician
5, physician
Luis Florián  5, neonatologist
5, neonatologist
Leidi Vilchez-Fernández
 6, neurologist
6, neurologist
Oscar Eguiluz-Loaiza
 6, neonatologist
6, neonatologist
Carmen Rosa Dávila-Aliaga
 3, neonatologist
3, neonatologist
Pilar Medina-Alva
 1,3, Pediatric neurologist
1,3, Pediatric neurologist
1 Universidad
Peruana Cayetano Heredia, Lima, Perú.
2 Hospital Cayetano Heredia, Lima, Perú.
3
Instituto Nacional Materno Perinatal, Lima, Perú.
4 Hospital
Nacional Docente Madre Niño San Bartolomé, Lima, Perú.
5
Hospital Nacional Arzobispo Loayza, Lima, Perú.
6 Hospital
Nacional Daniel Alcides Carrión, Lima, Perú.
7 Hospital
Nacional Guillermo Almenara Irigoyen, Lima, Perú.
ABSTRACT
Objective: To
determine the incidence and the clinical, bacteriological and cerebrospinal
fluid characteristics of neonatal meningitis in Lima hospitals.
Materials and methods:
An observational, multicenter study was conducted in six hospitals in the city
of Lima during 1 year of epidemiological surveillance.
Results: The cumulative
hospital incidence was 1.4 cases per 1000 live births. A total of 53 cases of
neonatal meningitis were included, 34% (18/53) were early and 66% (35/53) late.
The associated maternal factors were meconium-stained amniotic fluid and urinary
tract infection. Insufficient prenatal check-ups were found in 58.8% (30/51).
The most associated neonatal factor was sepsis. The main symptoms were fever,
irritability, hypoactivity and respiratory distress. Pleocytosis in
cerebrospinal fluid (CSF) was significant, without predominance of
polymorphonuclear lymphocytes (PMN), hypoglycorrhagia and proteinorrhagia. The
most frequent pathogens isolated were Escherichia coli and Listeria
monocytogenes.
Conclusions: The
hospital incidence of neonatal meningitis was 1.4 per 1000 live births, being
ten times higher in preterm infants. Breathing difficulty was the most frequent
symptom in the early stage, while fever and irritability in the late stage. CSF
showed pleocytosis without predominance of PMN. The most frequent germs were
Escherichia coli and Listeria monocytogenes. Ventriculitis and
hydrocephalus were the most common neurological complications.
Keywords:
Meningitis; Newborn; Premature; Cerebrospinal Fluid; Peru (source: MeSH
NLM).
INTRODUCTION
Neonatal
meningitis (NM) is a devastating disease, known to exist for over a century.
Early publications emphasized its clinical rarity and cumbersome diagnostic
process (1,2). However, over time it has
been reported on every continent, and despite scientific and technological
advances, it remains a public health problem (3).
Incidence
of NM varies considerably. In developed countries, it is estimated to be around
0.3 cases per 1,000 live births, while in developing countries this incidence
can be as high as 6.1 cases per 1,000 live births (3). With the new
methods, detection has improved and lethality has decreased; however, morbidity
remains high (20-60%) (4).
In
Peru, Oliveros reported 0.47 cases per 1,000 live births in 1993 (6).
However, in recent years an upward trend has been observed, ranging from 0.9 to
1.5 cases per 1,000 live births (5-7). This incidence could be
greater in our population due to the high frequency of maternal-perinatal
factors, such as insufficient prenatal control, sepsis, immaturity due to
prematurity and factors inherent to neonatal intensive care (5).
NM is
classified in 2 types, early and late (8). Early NM starts within
the first 72 hours and is related to contamination through the birth canal with
bacteria such as Escherichia coli, Streptococcus group B and Listeria
monocytogenes (9,10). After 72 hours,
late NM is associated with germs from the hospital environment, such as
coagulase-negative Staphylococcus and gram-negative bacilli (Escherichia
coli, Klebsiella pneumoniae, Enterobacter
spp.) (9-11).
NM is
a health emergency, and as soon as it is suspected, empirical antibiotic
treatment should be indicated (12). However, diagnosis is complex
due to the low specificity of signs and symptoms and the difficulty of
isolating the germs by culture. So, when risk factors are detected, clinical
suspicion is the only alternative (2,8).
Given
the scarce information on NM in our country regarding aspects such as its
frequency, impact on morbimortality and the prevalence of the pathogens
involved (9,12), it is extremely important to know the
epidemiological and clinical profile of the disease. For this reason, the
objective of the study was to estimate the incidence, associated factors,
clinical aspects and cerebrospinal fluid (CSF) characteristics, etiology, and
complications of NM in hospitals in the city of Lima.
|
KEY
MESSAGES
|
|
Motivation
for the study:
The frequency of neonatal meningitis in some
hospitals and the absence of a treatment protocol motivated an
epidemiological surveillance study in Lima.
Main
findings: An incidence of 1.4 cases per 1,000 live births was found, preterm infants represented the highest proportion.
Symptoms were non-specific, mainly respiratory distress in early NM, and
fever and irritability in the late type. Cerebrospinal fluid showed moderate pleocytosis with hypoglycorrhachia
and hyperproteinorrhachia. Escherichia coli
and Listeria monocytogenes predominated.
Implications: There is a need
to standardize the diagnostic and treatment criteria for NM. Likewise,
epidemiological surveillance should continue in the neonatal units of our
country.
|
MATERIALS AND METHODS
Design and population
Multi-center
case series study carried out between 2017 and 2018, with the aim of carrying
out hospital epidemiological surveillance of NM for 12 consecutive months in
Lima hospitals, without intervening in the diagnosis and treatment processes.
To be
included in the study, hospitals had to have neonatal units, neonatal
physicians, specialized nursing staff, specialists in neurology or neuropediatrics, neuroimaging equipment and a clinical
laboratory suitable for processing general analysis and cytochemical and
bacteriological examination of CSF. For this purpose, 12 hospitals were
selected, from which 6 met the inclusion criteria: Hospital Cayetano Heredia
(HCH), Hospital Nacional Docente Madre Niño San Bartolomé
(HSB), Hospital Nacional Arzobispo Loayza (HNAL), Instituto Nacional
Materno Perinatal (INMP), Hospital Nacional Guillermo
Almenara Irigoyen (HNGAI) and Hospital Nacional
Daniel Alcides Carrión
(HNDAC). All were level III health facilities.
A
research team was organized with physicians representing each of the six
hospitals, who were trained in the process of inclusion, follow-up and
collection of clinical and laboratory data. All centers had a neonatologist and
a neurologist. A new-case alert system was developed. The possibility of a
case, was recorded, communicated and confirmed by the representant of each
hospital. The monitoring and data collection continued until discharge. An ad
hoc clinical file was created, with data about filiation, sex, age,
gestational age, prenatal, birth and postnatal data, CSF characteristics and
bacteriological data. There was no interference in management decisions. In all
hospitals the objectives of the project were presented to the pediatric medical
team.
In
order to estimate hospital incidents, the number of births during the
observation period was recorded, according to the perinatal register and
statistics office of each hospital. Finally, premature births were recorded by
gestational age and sex.
Variables
All full-term
infants under 28 days or pre-term infants under 44 weeks corrected gestational age
were entered into the study. The inclusion criteria for all cases of NM were
infants who were symptomatic or at risk of infection; pleocytosis
≥ 30 leukocytes/μL in CSF, diagnosis and care at the
hospital of birth. The hospital follow-up concluded with the discharge of the
patient. Neonates with severe cerebral malformations and spinal dysraphism were
excluded.
NM categorization
was confirmed (germ identified), probable (high bacterial suspicion), and
possible (low bacterial suspicion) (5,11).
NM was confirmed when the germ was identified in the CSF, by culture,
polymerase chain reaction (PCR), coagglutination or
blood culture. Probable NM was defined by hypoglycorrhachia (glycorrhachia ≤50%
of serum glucose or absolute glycorrhachia of ≤40 mg/dL) and hyperproteinuria
(proteinuria ≥60 mg/dL) (5,8). Cases of possible NM had any level of glycorrhachia or proteinorrhachia
or normal biochemical values. The viruses were identified by PCR or viral indirect
immunofluorescence (viral IIF) in the CSF. The fungi were identified by CSF
culture/PCR. In the case of lumbar punctures (LP), a leukocyte was discounted
for every 500 red blood cells in CSF.
Early
MN was defined as, confirmed, probable or possible cases diagnosed before 72
hours of age. Late NM was defined as cases diagnosed after 72 hours of
age (5,8). Early neurological
complications were defined within the first seven days of detection. The
complications considered were hydrocephalus, ventriculitis, subdural effusion
and cerebral infarction, identified by cerebral ultrasound or cerebral magnetic
resonance.
In
order to measure the burden of disease, out-of-hospital cases were recorded.
Out-of-hospital cases are defined as cases of NM born in other hospitals and
admitted during the study period.
A set
of prenatal, natal and postnatal variables were recorded and analyzed. Numerical
variables were: maternal age, antenatal control, gestational age, birth weight;
and categorical variables were: maternal urinary infection, maternal fever,
chorioamnionitis, presence of meconium amniotic fluid, pre-eclampsia /
eclampsia, asphyxia, intraventricular hemorrhage, sepsis, anemia, meconium
aspiration, fever, respiratory distress, hypoactivity, irritability, vomiting.
Likewise, CSF characteristics and germ frequencies, treatment, complications
and lethality were recorded and analyzed.
Ethical considerations
The
identity of the patients was protected by numerical codes. The project was also
approved by the Institutional Ethics Committee of Universidad Peruana Cayetano
Heredia and by the ethics committees of each of the participating hospitals.
Statistical Analysis
The
information was collected and stored in a Microsoft Excel 2016 © database.
The accumulated incidence during one year of observation in each hospital was
determined. The project started in several successive months in 2017 and ended
sequentially in 2018. The cumulative incidence was estimated from the sum of
confirmed cases, probable cases and possible cases divided by the number of
live births. Out-of-hospital cases were not considered for the incidence
calculation.
The
frequencies of clinical and laboratorial variables are presented for early,
late and out-of-hospital NM. Numerical variables were summarized with medians
and their interquartile range. Logistic regression was performed to determine
the influence of some factors on early meningitis with respect to late
meningitis, by analyzing all cases. Homogeneity was determined by the Levene and Forsythe-Browne tests. The only few missing data
were from the prenatal control variable, so no replacement technique was
necessary.
RESULTS
Patient Enrollment
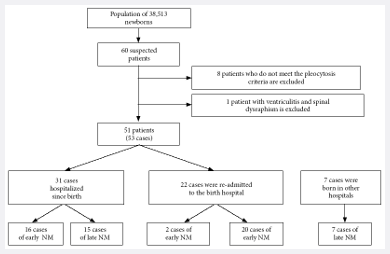
The
project started in 2017. Given that the enrollment in hospitals was carried out
gradually, the study was completed in 2018. During this period a total of
38,513 live neonates were registered in the six hospitals, of which 51 patients
were included who developed 53 cases of NM, one patient presented three
episodes of NM. From the reported cases, 41.5% (22/53) were neonates who,
having left the hospital in good condition, were readmitted on suspicion of an
infectious process. During the study period, seven out-of-hospital cases were
admitted (Figure
1), considered only for the profile of clinical, etiological
and laboratorial analysis.
NM: neonatal meningitis
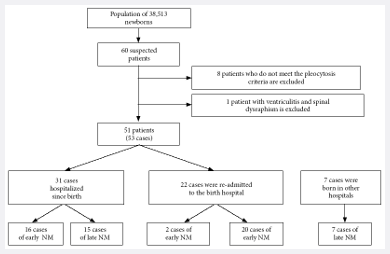
Figure 1. Patient
flow chart.
The
average maternal age was 27.2 years and parity was 2.3 per woman. The number of
prenatal controls was also insufficient in 58.8% (30/51) of the mothers. From
the neonates, 54.7% (29/53) were born prematurely before 37 weeks. The
population studied was homogeneous among the hospitals included.
Epidemiological
characteristics
The
hospital incidence was 1.4 cases per 1,000 live births, with a wide variation
among hospitals, from 0 to 3.2 cases per 1,000 live births. HCH and HNDMNSB had
the highest incidence. In pre-term infants under 37 weeks, the NM incidence was
7.5 cases per 1,000 live births and 0.7 cases per 1,000 live full-term births
(Table 1).
Table 1. Cumulative incidence of neonatal meningitis according
to hospital institution
|
Institution |
Total |
Pre-term |
|
Live births |
Cases |
Cumulative incidence (per 1,000 live births) |
Live births |
Cases |
Cumulative incidence (per 1,000 live births) |
|
Hospital Nacional Cayetano Heredia |
4,436 |
14 |
3.2 |
826 |
7 |
8.5 |
|
Hospital Nacional Docente Madre
Niño San Bartolomé |
6,155 |
20 |
3.2 |
395 |
8 |
20.3 |
|
Instituto Nacional Materno Perinatal |
18,138 |
17 |
0.9 |
1,634 |
13 |
8.0 |
|
Hospital Nacional Arzobispo Loayza |
2,765 |
1 |
0.4 |
226 |
0 |
0.0 |
|
Hospital Nacional Daniel Alcides Carrión |
3,915 |
1 |
0.3 |
481 |
1 |
2.1 |
|
Hospital Guillermo Almenara Irigoyen |
3,104 |
0 |
0.0 |
280 |
0 |
0.0 |
|
Total |
38,513 |
53 |
1.4 |
3,842 |
29 |
7.5 |
Surveillance during a 1-year period.
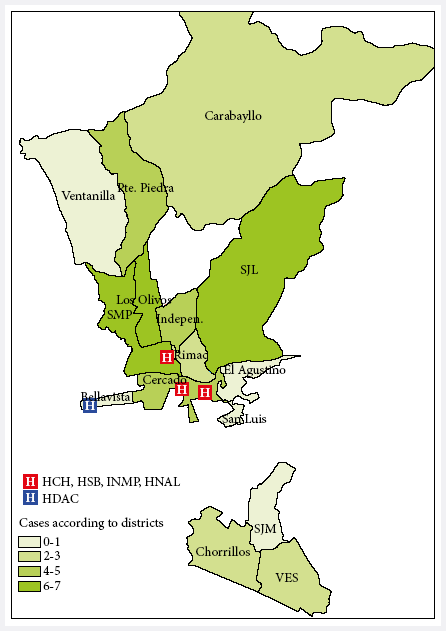
The male/female ratio was 1.4; males represented the 58.3% (35/60) and
females 41.7% (25/60). The majority of patients were from northern Lima at 42%
(25/60), mainly from the districts of San Martín de Porres
and Los Olivos, followed by districts of eastern Lima
at 15% (9/60).
Figure 2 shows that the cases came from areas surrounding the
hospitals.
HCH: Hospital Cayetano Heredia
HSB: Hospital San Bartolomé
HNAL: Hospital Nacional Arzobispo Loayza
HDAC: Hospital Daniel Alcides Carrión
INMP: Instituto Nacional Materno Perinatal
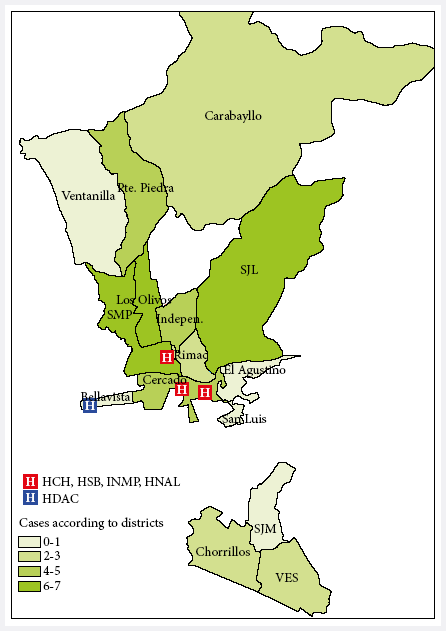
Figure 2.
Distribution of neonatal meningitis cases by district of origin (Metropolitan
Lima)
From the total, 34% (18/53) were early NM cases and 66% (35/53) were late
NM cases. Cases of confirmed NM were 58.5% (31/53), of which 25.8% (8/31) were
early and 74.2% (23/31) late. Bacterial NM occurred in 87.1% (27/31) of the
confirmed cases and viral NM in 12.9% (4/31). Probable NM was 22.6% (12/53) of
the total of cases and possible NM was 18.9% (10/53). Regarding outpatients, 4
had confirmed NM, 2 had probable NM and 1 had possible NM.
Clinical
characteristics
For early NM, the associated prenatal factors were meconial amniotic
fluid (38.9%), urinary tract infection (33.3%), maternal fever (27.8) and
chorioamnionitis (22.2%). However, in the late NM, these factors did not seem
to have a major influence (Table 2).
Table 2.
Prenatal, natal and postnatal characteristics, according to the type of
meningitis
|
Characteristic |
Early NM (n = 18) |
Late NM (n = 35) |
Out-of-hospital NM (n = 7) |
|
n (%) |
n (%) |
n (%) |
|
Cesarean section delivery |
11 (61.1) |
18 (51.4) |
3 (42.9) |
|
Prenatal controls |
|
|
|
|
<6 |
10 (55.5) |
17 (54.8) |
3 (42.9) |
|
6 or more |
4 (22.3) |
14 (45.2) |
3 (42.9) |
|
Prenatal and natal factors |
|
|
|
|
Medications during pregnancy |
0 (0.0) |
1 (2.9) |
1 (14.3) |
|
Maternal fever |
5 (27.8) |
1 (2.9) |
0 (0.0) |
|
Premature rupture of membranes >18 h |
3 (16.7) |
9 (25.7) |
0 (0.0) |
|
Urinary tract infection |
6 (33.3) |
7 (20.0) |
2 (28.6) |
|
Vaginal infection |
0 (0.0) |
2 (5.7) |
1 (14.3) |
|
Pelvic-uterine surgery |
1 (5.6) |
0 (0.0) |
0 (0.0) |
|
Meconium-stained amniotic fluid |
7 (38.9) |
9 (25.7) |
1 (14.3) |
|
Chorioamnionitis |
4 (22.2) |
5 (14.3) |
0 (0.0) |
|
Prolonged labor |
2 (11.1) |
1 (2.9) |
0 (0.0) |
|
Preeclampsia/eclampsia |
2 (11.1) |
5 (14.3) |
1 (14.3) |
|
Intrauterine growth restriction |
0 (0.0) |
2 (5.7) |
0 (0.0) |
|
Male gender |
11 (61.1) |
20 (57.1) |
4 (57.1) |
|
Gestational age (weeks) |
|
|
|
|
<37 |
11 (61.1) |
18 (51.4) |
3 (42.9) |
|
≥37 |
7 (38.9) |
17 (48.6) |
4 (57.1) |
|
Weight (grams) |
|
|
|
|
<1,500 |
4 (22.2) |
9 (25.7) |
2 (28.6) |
|
1,500 to 2,499 |
7 (38.9) |
10 (28.6) |
1 (14.3) |
|
≥2,500 |
7 (38.9) |
16 (45.7) |
4 (57.1) |
|
Age at the onset of symptoms (days)
a |
0.9 (1.8) |
18.6 (20.1) |
11.9 (11.6) |
|
Postnatal factors |
|
|
|
|
Sepsis |
9 (50.0) |
7 (20.0) |
3 (42.9) |
|
Asphyxia |
1 (5.6) |
0 (0.0) |
2 (28.6) |
|
Meconium aspiration |
0 (0.0) |
1 (2.9) |
1 (14.3) |
|
Intraventricular hemorrhage |
4 (22.2) |
2 (5.7) |
1 (14.3) |
|
Anemia |
0 (0.0) |
1 (2.9) |
0 (0.0) |
|
Connatal pneumonia |
1 (5.6) |
0 (0.0) |
0 (0.0) |
|
Pathological jaundice |
0 (0.0) |
0 (0.0) |
1 (14.3) |
|
Symptoms |
|
|
|
|
Fever |
7 (38.9) |
19 (54.3) |
5 (71.4) |
|
Irritability |
7 (38.9) |
20 (57.1) |
3 (42.9) |
|
Hypoactivity |
7 (38.9) |
17 (48.6) |
4 (57.1) |
|
Breathing difficulty |
13 (72.2) |
10 (28.6) |
3 (42.9) |
|
Weak sucking |
4 (22.2) |
12 (34.3) |
3 (42.9) |
|
Vomiting |
1 (5.6) |
2 (5.7) |
4 (57.1) |
|
Jaundice |
4 (22.2) |
4 (11.4) |
5 (71.4) |
|
Apnea |
5 (27.8) |
7 (20.0) |
1 (14.3) |
|
Convulsions |
2 (11.1) |
6 (17.1) |
1 (14.3) |
|
Bulging fontanelle |
3 (16.7) |
2 (5.7) |
3 (42.9) |
|
Hypotonia |
5 (27.8) |
6 (17.1) |
3 (42.9) |
|
Hypertonia |
3 (16.7) |
2 (5.7) |
2 (28.6) |
|
Hyperreflexia |
1 (5.6) |
3 (8.6) |
1 (14.3) |
|
Hyporreflexia |
2 (11.1) |
1 (2.9) |
2 (28.6) |
|
Lethality |
1 (5.6) |
1 (2.9) |
0 (0.0) |
NM: neonatal meningitis
a Mean (SD)
Sepsis was the most important factor related to NM; and according to the
NM types, 50% (9/18) were early meningitis cases, 20% (7/35) were late
meningitis cases and 42.9% (3/7) were of out-of-hospital meningitis cases. The average
age for the onset of symptoms in early NM cases was 0.9 days; 18.6 days in late
NM; and 11.9 days in the out-of-hospital cases. Symptoms such as respiratory distress, were more common in the early NM. In late NM,
fever, irritability and hypoactivity predominated (Table 2). Table 5 shows the
risk factors associated with early NM in relation to late NM.
Table 5. Factors associated with early neonatal meningitis compared to late
neonatal meningitis.
|
Factor |
OR |
p-value |
95% CI |
|
Maternal fever |
18.51 |
0.021 |
1.56-219.87 |
|
Sepsis |
5.10 |
0.040 |
1.08-24.07 |
|
Breathing difficulty |
4.59 |
0.043 |
1.05-20.11 |
|
Cesarean section delivery |
4.12 |
0.079 |
0.85-20.01 |
OR: Odds Ratio, 95% CI: 95% confidence interval
Cytochemical and bacteriological
characteristics of the CSF
On average, 2.5 and 2 LPs were performed for early and late NM,
respectively. In most cases of early NM, the LP was performed on the first day
of hospitalization; and in cases of late NM, it could take until the third day
of illness.
In
Table 3, the cytochemical characteristics of the CSF are presented.
The median value for pleocytosis was 225 leukocytes/μL for early NM
and 202 leukocytes/μL for late NM, the median value
for polymorphonuclears (PMN) was of 57% and 30%, respectively. Hypoglycorrhachia
was similar in both types of meningitis and hyperproteinorrhachia
was higher in early NM. In the out-of-hospital type, there was less pleocytosis and more glycorrhachia
(
Table 3).
Table 3.
Cerebrospinal fluid characteristics, according to the
type of meningitis.
|
Variable |
Early NM (n = 18) |
Late NM (n = 35) |
Out-of-hospital NM (n = 7) |
|
Median |
IQR |
Median |
IQR |
Median |
IQR |
|
Leucocytes (cells/μL) |
225 |
130-1912 |
202 |
45-530 |
150 |
32-866 |
|
PMN (%) |
57 |
30-70 |
30 |
10-52 |
60 |
35-60 |
|
Glucose (mg/dL) |
36 |
24-42 |
32 |
25-44 |
43 |
34-46 |
|
Proteins (mg/dL) |
188 |
115-499 |
125 |
81-201 |
139 |
62-266 |
|
Erythrocytes (cells/μL) |
100 |
10-500 |
3 |
0-100 |
32 |
5-50 |
NM: neonatal meningitis, IQR: interquartile range (25th and 75th
percentiles), PMN: polymorphonuclears
A total of 35 germs were identified, including bacteria, viruses
and a case of Candida albicans. In all clinical types, Escherichia
coli and Listeria monocytogenes predominated. In 17.1% (6/35) of the
cases the germ was isolated both in blood culture and in the CSF. Escherichia
coli was found in four of those cases, group B Streptococcus
and coagulase negative Staphylococcus, in one case each. Cases of
influenza B, coronavirus and adenovirus were identified by indirect
immunofluorescence (IIF). In a single case, PCR was performed, isolating herpes
virus VI (Table 4).
Table 4.
Isolation of the infectious agent according to the
type of meningitis.
|
Infectious agent |
Cultivated
fluid |
Early
NM |
Late
NM |
Out-of-hospital
NM |
Total |
|
Escherichia coli |
CSF |
3/18 |
2/35 |
0/7 |
10/60
a |
|
Blood |
2/18 |
7/35 |
0/7 |
|
Listeria monocytogenes |
CSF |
1/18 |
2/35 |
0/7 |
8/60 |
|
Blood |
3/18 |
2/35 |
0/7 |
|
Coagulase-negative Staphylococcus |
CSF |
0/18 |
1/35 |
1/7 |
3/60
a |
|
Blood |
1/18 |
1/35 |
0/7 |
|
Group B Streptococcus |
CSF |
0/18 |
1/35 |
1/7 |
2/60
a |
|
Blood |
0/18 |
0/35 |
1/7 |
|
Enterococo faecium |
CSF |
0/18 |
0/35 |
0/7 |
2/60 |
|
Blood |
1/18 |
1/35 |
0/7 |
|
Staphilococus epidermidis |
CSF |
0/18 |
0/35 |
0/7 |
2/60 |
|
Blood |
0/18 |
2/35 |
0/7 |
|
Serratia marcescens |
CSF |
0/18 |
0/35 |
0/7 |
1/60 |
|
Blood |
0/18 |
1/35 |
0/7 |
|
Serratia liquecies |
CSF |
0/18 |
0/35 |
0/7 |
1/60 |
|
Blood |
0/18 |
1/35 |
077 |
|
Staphilococus hominis |
CSF |
0/18 |
0/35 |
0/7 |
1/60 |
|
Blood |
0/18 |
0/35 |
1/7 |
|
Influenza B (IIF) |
CSF |
0/18 |
1/35 |
0/7 |
1/60 |
|
Adenovirus (IIF) |
CSF |
0/18 |
1/35 |
0/7 |
1/60 |
|
Coronavirus (IIF) |
CSF |
0/18 |
1/35 |
0/7 |
1/60 |
|
Herpes virus VI (PCR) |
CSF |
0/18 |
1/35 |
0/7 |
1/60 |
|
Candida albicans
(PCR) |
CSF |
0/18 |
0/35 |
0/7 |
1/60 |
|
Blood |
0/18 |
0/35 |
1/7 |
NM: neonatal meningitis; CSF:
cerebrospinal fluid; PCR: polymerase chain reaction; IIF: indirect
immunofluorescence
a
Isolation of the germ in both blood
and CSF
The total
represents the burden of disease addressed by all the hospitals.
Treatment
and special conditions
Treatment schedules were highly variable. The mean duration for cases of
early NM was 21 days and 19.5 days for late meningitis. Before the
first LP was performed, 62% of children received antibiotics. The most commonly
used drugs were ampicillin (60%), cefotaxime (38%), vancomycin (28%), meropenem
(33%) and gentamicin (22%), in different schedules.
In the specific analysis of late meningitis, not including outpatients,
two groups were differentiated (Figure 1). In the first group, 86.7% (13/15) of
patients were pre-term infants, 46.6% (7/15) had respiratory distress, most
were diagnosed at seven days of age, and their CSF was characterized by
increased pleocytosis. In the second group, 75% (15/20) were full-term infants,
fever and irritability were the most frequent symptoms and the diagnosis was
made within the first two days of hospitalization.
Three patients had special presentations. One had minor pleocytosis and
urinary-related bacteremia by Escherichia coli; another had normal
initial cytochemistry, but with a CSF culture positive for Escherichia coli
that later developed pleocytosis; and the third one had three episodes of
meningitis (recurrent) by extended-spectrum beta-lactamase-producing Escherichia
coli.
Complications
and lethality
At least one neurological complication was observed in 25% (15/60) of
the cases, from which, 73.3% (11/15) were pre-term infants. Early and late
neurological complications were ventriculitis and hydrocephalus respectively.
From the cases with late NM, 95.2% (40/42) were discharged with
favorable evolution, early NM had a favorable
evolution in 77.8% (14/18) of the cases. Four cases were referred to a hospital
with a higher complexity level. Two neonates died (3.3%), one presenting early
NM and the other, the late type.
DISCUSSION
NM had a hospital incidence of 1.4 cases per 1,000 live births, with a
higher risk in pre-term than in full-term infants. The wide variability in
incidence leads to the suspicion that diagnostic protocols for NM were not standarized across hospitals. A variety of causal germs,
mostly bacteria, were identified, with the frequency of Eschericha
coli and Listeria monocytogenes being particularly noteworthy.
We present a larger NM clinical scenario than those known. In this
scenario the early type is related to birth conditions and the late type is related
to prolonged stay of pre-term infants in neonatal units (9). We
provide a new viewpoint, derived from the community, which occurs more in
full-term infants near the second week, related to a higher proportion of viral
agents.
Neonatal meningitis is an under-diagnosed and under-recorded prevalent
disease in our country (5,13). In 2016, Zea et al., noted that LP is often deferred
in confirmed sepsis (14). Likewise, in a similar population it has
been observed that medical criteria may vary depending on the level of medical
specialization (15).
We present an epidemiological surveillance study according the
management protocols of each hospital. The incidence of 1.4 per 1,000 live
births is an average value worldwide (3), and is initially taken as a
reference. This value will have to be adjusted in the future when the
diagnostic criteria are standardized. However, the high incidence in premature
infants alerts us about the need for vigilance in neonatal units (2, 16).
This study was characterized by the inclusion of cases with defined pleocytosis. This was made to meet the inflammatory criteria for meningitis, classified
as confirmed, probable and possible, according to the definition of neonatal
sepsis. Therefore, more positive isolates were found in blood cultures. Less were found to be positive in blood and CSF cultures, and
only a few cases were observed solely in CSF culture. We believe that PCR could have helped to reduce
the number of probable and possible cases, and to identify cases of pleocytosis
as just an inflammatory phenomenon (8,9,17).
All known risk factors for neonatal sepsis are related to NM (12,18). For the early type, peripartum fever and
incomplete prenatal controls were found to be risk factors. These factors
suggest the risk of microbial invasion from the vaginal flora, the subsequent
placental inflammatory response, initiation of labor and consequently sepsis
and meningitis (8). However, other clinical and sociocultural
factors may not be considered.
Classically, NM is divided into early and late according to its
mechanism of contamination (12,16,19).
However, we have identified a third group of patients who come from their
homes, from the community environment, are term infants, febrile and irritable
with less pleocytosis, contaminated with common respiratory tract agents, both
bacterial and viral, and in some cases by germs that colonize maternal
secretions.
The age of symptoms onset for both types of NM was found to be within
the expected ranges, 0.9 days for early NM cases and 18.6 days for late NM
cases. This was found to be in accordance with other series, and clearly
associated with the type of birth and neonatal unit stay (12,16,20). The group of children of out-of-hospital
origin also behaved as late NM at 11.9 days.
The symptoms were more frequent in early NM than in the late type, being
very nonspecific and related to sepsis. Among them, respiratory difficulty
stood out in 70% of early cases, perhaps due to lung immaturity in the
premature group or to respiratory acidosis (3,12,16).
In late NM more neurological symptoms were observed (1,3).
However, identification of these symptoms depends on the experience of the
examiner (14,21). Maternal fever, sepsis,
and respiratory distress were three factors found to be more likely to develop
in early NM than in the late type. These were probably generated by maternal
infections, urinary tract infections and chorioamnionitis (1,8). It will remain for future studies to ensure the
diagnosis of chorioamnionitis by pathological examination of the placenta.
In most cases, more than one LP was carried out, following international
guidelines. Given that NM is a difficult to diagnose multi-symptomatic disease
caused by many aggressive agents, the guidelines recommend that the LP be
performed prior to the use of antibiotics. It is also recommended that a new control
should be performed within 48-72 hours, especially if there is no clinical
improvement, with the purpose of reducing the bacterial load or achieving sterilization
of the CSF (14,21,22).
In both clinical types, moderate pleocytosis without PMN predominance
was noted, they also presented hypoglycorrhachia and proteinorrhachia. This particular characteristic has
already been observed in other national studies (6,7),
perhaps, bacteriological factors, sample processing and patient’s immunological
conditions are involved. In bacterial NM, hypoglycorrhachia
and proteinorrhachia are common findings. These are explained
by glucose consumption and increased detritus, their persistence for more than
two weeks has been associated with poor prognosis (23). However,
these indicators may be aggravated by the presence of intracranial hemorrhage.
Also, on rare occasions, the first LP may not demonstrate pleocytosis, and a
second sample may be required within 12 to 24 hours (21).
The microbiological behavior of NM has varied regarding time and
different geographical areas (2,3,16,24-26).
Streptococcus agalactie stands out mainly in
developed countries and gram‑negative bacteria in non‑developed countries (3,24). In this series, Eschericha
coli and Listeria monocytogenes were the prevalent germs in both types
of NM, followed by a variety of gram‑negative and gram‑positive bacteria, fewer
virus cases and one case of Candida albicans, all described in different
case series.
NM by Eschericha coli has been
known for many decades (1,2) to be a part
of early neonatal sepsis cases. It can also cause late NM, usually associated
with severe acute and mid‑term complications such as hydrocephalus, subdural
effusions, cerebral infarctions and abscesses (2,27).
In recent years, the increased frequency of beta‑lactamase strains and their
antimicrobial resistance has being notable (24,26).
Therefore, their presence in this series alerts about early identification and
treatment.
Listeria monocytogenes is a pathogen that has become
more important in Peruvian series in recent years (5,7).
It has been observed to be 5-20% (26) of the early and late types
reported, and it usually produces a moderate or severe disease, according to
some international and national reports. However, its infectious mechanism is
not clearly identified, but it is understood that the invasion is by
genitourinary route and related to the maternal intestinal flora.
The lethality rate by NM in national reports has been decreasing over
time. In 1993, Oliveros et al. reported 20% death in a series
of 24 cases (6), and in 2017, Lewis reported 3.8% in a series of 53
patients (5). Such decrease may be related to early diagnosis and
treatment. However, the frequency of neurological complications was 25%, and
the high morbidity in premature infants (75%) was noteworthy (28,29). Consequently, the use of cerebral ultrasound as
a diagnostic tool for hydrocephalus, ventriculitis and cerebral infarction is
very important in premature infants (30).
Not including certain variables such as prenatal steroid use,
intrauterine infections, histological chorioamnionitis, invasive procedures,
recording of sepsis cases without meningitis, antimicrobial sensitivity and
resistance, community contacts, and not involving more hospitals are among the
main limitations of this study. However, the strengths of the study were to
demonstrate that NM is frequent, that pre-term infants are at greater risk,
that the disease can present itself in different ways and that a wide spectrum
of causal infectious agents exists. With these considerations we contribute to
the national knowledge of this disease.
In conclusion, the hospital incidence of NM was 1.4 cases per 1,000 live
births, and even higher in premature infants. Respiratory distress was the most
frequent symptom for early NM, while fever and irritability were the most
frequent symptoms of late NM. Moderate pleocytosis,
with hypoglycorrhachia and proteinorrhachia,
was noted in the CSF. The most frequent pathogens isolated were Eschericha coli and Listeria monocytogenes.
The most common neurological complications were ventriculitis and
hydrocephalus. A new pathogenic scenario for NM is proposed, it consists of
three infection types: vertical infection, by vaginal flora germs; nosocomial
infection, by contamination in neonatal units; and infection from the community
by common germs.
A national epidemiological surveillance study of NM is recommended. This
study should standardize diagnostic criteria (clinical, cytochemical, culture, PCR),
neuroimaging criteria (ultrasound and resonance) and criteria for
identification of perinatal risk factors.
Acknowledgement:
To all physicians and nurses in the neonatal departments of the
participating hospitals.
REFERENCES
1. Bell WE, McCormick
WF, Murillo PL. Meningitis neonatales. Infecciones neurológicas en el
niño. 2a ed. Barcelona: Salvat; 1979.
2. Ziai M, Haggerty RJ.
Neonatal meningitis. N Engl J Med. 1958;259(7):314-20. doi:
10.1056/NEJM195808142590702.
3. Ku LC, Boggess KA,
Cohen-Wolkowiez M. Bacterial Meningitis in the Infant. Clin Perinatol.
2015;42(1):29–45. doi: 10.1016/j.clp.2014.10.004.
4. Holt DE. Neonatal
meningitis in England and Wales: 10 years on. Arch Dis Child - Fetal
Neonatal Ed. 2001;84(2):85F-89.
5. Lewis G, Schweig M, Guillén-Pinto D, Rospigliosi ML.
Meningitis neonatal en un hospital general de Lima, Perú, 2008 al 2015. Rev
Peru Med Exp Salud Pública. 2017; 34:233-8. doi:
10.17843/rpmesp.2017.342.2297.
6. Oliveros Donohue MA,
Ramos Pianezzi R, León Cueto JL, Mazzini Pérez-Reyes J, Van Oordt,
Bellido J, Livia Becerra C. Meningitis neonatal en la UCI del Hospital
Edgardo Rebagliati Martins (IPSS) 1986-88. Diagnóstico.
1993;32(4/6):73-7.
7. Lazo E, Guillén D, Zegarra J. Meningitis neonatal
en el Hospital Nacional Cayetano Heredia. Rev Peru Pediatr.
2008;61(3):157-164.
8. Volpe J. Bacterial and Fungal Intracranial
Infections. Neurology of the Newborn. Fifth Edition. Philadelphia:
Saunders Elsevier; 2013.
9. Devi U, Bora R,
Malik V, Deori R, Gogoi B, Das JK, Mahanta J. Bacterial aetiology of
neonatal meningitis: A study from north-east India. Indian J Med Res.
2017 Jan;145(1):138-143. doi: 10.4103/ijmr.IJMR_748_15.
10. Pérez RO, Lona JC,
Quiles M, Verdugo MÁ, 4Ascencio EP, Benítez EA. Sepsis neonatal temprana,
incidencia y factores de riesgo asociados en un hospital público del
occidente de México. Rev Chil Infectol. 2015;32(4):447-452.
11. Zea-Vera A, Turin CG, Ochoa TJ. Unificando los
criterios de sepsis neonatal tardía: propuesta de un algoritmo de
vigilancia diagnóstica. Rev Peru Med Exp Salud Pública.
2014;31(2):358-63.
12. Perlman JM, Cilio M. Neonatal Meningitis: Current
Treatment Options. Neurology. Neonatology Questions and Controversies.
Third Edition. Phyladelphia: Elsevier; 2019.
13. Medina, María del Pilar. Frecuencia de enfermedad
neurológica en recién nacidos. Rev Peru Pediatr. 2007;60(1):11-9.
14. Zea-Vera A, Turín CG, Rueda MS, Guillén-Pinto D.
Uso de la punción lumbar en la evaluación de sepsis neonatal tardía en
recién nacidos de bajo peso. Rev Peru Med Exp Salud Pública.
2016;33(2):278-282.
15. Vera S.
Variabilidad del criterio para indicar la punción lumbar en las unidades
de cuidados intensivos neonatales [tesis de bachiller]. Lima: Facultad
de Medicina, Universidad Peruana Cayetano Heredia; 2018.
16. Coto GD, López JB,
Fernández B, Fraga JM, Fernández JR, Reparaz R, et al. Meningitis
neonatal. Estudio epidemiológico del Grupo de Hospitales Castrillo. An
Pediatr. 2002;56(6):556-63.
17. Marcilla C, Martínez A, Carrascosa M, Baquero M,
Alfaro B. Meningitis víricas neonatales. Importancia de la reacción en
cadena de la polimerasa en su diagnóstico. Rev Neurol. 2018; 67:484-490.
18. Shane AL, Sánchez
PJ, Stoll BJ. Neonatal sepsis. Lancet. 2017;390(10104):1770-80. doi:
10.1016/S0140-6736(17)31002-4.
19. Zhao Z, Yu J-L,
Zhang H-B, Li J-H, Li Z-K. Five-Year Multicenter Study of Clinical Tests
of Neonatal Purulent Meningitis. Clin Pediatr (Phila).
2018;57(4):389–97. doi: 10.1177/0009922817728699.
20. Olmedo I, Pallas
CR, Miralles M, Simón de las Heras R, Rodriguez J, Chasco A. Meningitis
neonatal: Estudio en 56 casos. An Esp Pediatr. 1997; 46:189-194.
21. Garges HP. Neonatal
Meningitis: What Is the Correlation Among Cerebrospinal Fluid Cultures,
Blood Cultures, and Cerebrospinal Fluid Parameters? Pediatrics.
2006;117(4):1094–100.
22. Greenberg RG, Benjamin DK, Cohen-Wolkowiez M,
Clark RH, Cotten CM, Laughon M, et al. Repeat lumbar punctures in
infants with meningitis in the neonatal intensive care unit. J
Perinatol. 2011;31(6):425–429. doi: 10.1038/jp.2010.142.
23. Tan J, Kan J, Qiu G, Zhao D, Ren F, Luo Z, Zhang
Y. Clinical Prognosis in Neonatal Bacterial Meningitis: The Role of
Cerebrospinal Fluid Protein. PLoS One. 2015 Oct 28;10(10):e0141620. doi:
10.1371/journal.pone.0141620.
24. Collaborative Study
Group for Neonatal Bacterial Meningitis. A multicenter epidemiological
study of neonatal bacterial meningitis in parts of South China. Zhonghua
Er Ke Za Zhi Chin J Pediatr. 2018;56(6):421–428. doi:
10.3760/cma.j.issn.0578-1310.2018.06.004.
25. Berardi A , Lugli L
, Rossi C , China MC , Vellani G , Contiero R , et al. Infezioni
da Streptococco B Della Regione Emilia Romagna . Neonatal bacterial
meningitis. Minerva Pediatr. 2010;62(3 Suppl 1):51-4.
26. Bentlin MR,
Ferreira GL, Rugolo LMS de S, Silva GHS, Mondelli AL, Rugolo Júnior A.
Neonatal meningitis according to the microbiological diagnosis: a decade
of experience in a tertiary center. Arq Neuropsiquiatr.
2010;68(6):882–887.
27. Zhu M-L, Mai J-Y, Zhu J-H, Lin Z-L. Clinical
analysis of 31 cases of neonatal purulent meningitis caused by
Escherichia coli. Zhongguo Dang Dai Er Ke Za Zhi Chin J Contemp
Pediatr. 2012;14(12):910–912.
28. Ouchenir L, Renaud C, Khan S, Bitnun A, Boisvert
A-A, McDonald J, et al. The Epidemiology, Management, and
Outcomes of Bacterial Meningitis in Infants. Pediatrics.
2017;140(1):1-8. Pediatrics. 2017 Jul;140(1). doi:
10.1542/peds.2017-0476.
29. Krebs VLJ, Costa
GAM. Clinical outcome of neonatal bacterial meningitis according to
birth weight. Arq Neuropsiquiatr. 2007;65(4b):1149–1153.
30. Gupta N, Grover H, Bansal I, Hooda K, Sapire JM,
Anand R, Kumar Y. Neonatal cranial sonography: ultrasound findings
in neonatal meningitis-a pictorial review. Quant Imaging Med Surg. 2017
Feb;7(1):123-131. doi: 10.21037/qims.2017.02.01.
Citation:
Guillén-Pinto D, Málaga-Espinoza B, Ye-Tay J, Rospigliosi-López ML,
Montenegro-Rivera A, Rivas M, et al.
Neonatal
meningitis: a multicenter study in Lima, Peru. Rev Peru
Med Exp Salud Publica. 2020;37(2):210-9. doi:
https://doi.org/10.17843/rpmesp.2020.372.4772
Correspondence to:
Daniel Guillén Pinto; Av. Honorio Delgado
430, Urb. Ingeniería, San Martín de Porres, Lima, Perú;
dgu4illenpinto@gmail.com.
Funding:
This research was entirely self-financed.
Authors’ contributions:
DGP participated in the
conception of this study. DGP, BM and JY participated in the study design,
writing and data analysis. BM and JY participated in the enrollment and data
collection. MLR, AM, MR, MLS, SV, OL, AT, LC, LF, LV, OE, CD and PM
participated in the data collection. All authors reviewed and approved the
article.
Conflict of interest:
The authors declare no
conflict of interest.
Received: 30/08/2019
Approved:
29/04/2020
Online: 15/06/2020
![]() 1,2, Pediatric neurologist
1,2, Pediatric neurologist![]() 1, physician
1, physician![]() 1, physician
1, physician![]() 1,2, neonatologist
1,2, neonatologist![]() 1, pediatrician
1, pediatrician![]() 4, Pediatric neurologist
4, Pediatric neurologist![]() 4, Pediatric neurologist
4, Pediatric neurologist![]() 4, neonatologist
4, neonatologist![]() 7, neonatologist
7, neonatologist![]() 7, Pediatric neurologist
7, Pediatric neurologist![]() 5, physician
5, physician![]() 5, neonatologist
5, neonatologist![]() 6, neurologist
6, neurologist![]() 6, neonatologist
6, neonatologist![]() 3, neonatologist
3, neonatologist![]() 1,3, Pediatric neurologist
1,3, Pediatric neurologist