Eduardo Falconí-Rosadio
Joshi Acosta
ORIGINAL ARTICLE
Interpretation systems, therapeutic itineraries and repertoires
of leprosy patients in a low prevalence country
Carmen Osorio-Mejía
![]() 1,
Microbiological biologist,
Public Health specialist
1,
Microbiological biologist,
Public Health specialist
Eduardo Falconí-Rosadio
![]() 1, Infectologist and Tropical
Medicine specialist
1, Infectologist and Tropical
Medicine specialist
Joshi Acosta
![]() 2, Medical microbiologist, doctor
of Microbiology
2, Medical microbiologist, doctor
of Microbiology
1 Instituto
Nacional de Salud, Lima, Peru.
2 Instituto de
Evaluación de Tecnologías en Salud e Investigación, ESSALUD, Lima, Peru.
ABSTRACT
Objectives: In Peru, despite the small number of cases, there is evidence
of late diagnosis and hidden
Materials and methods: A qualitative study was carried out, applying semi-structured
interviews to patients diagnosed with leprosy from the Loreto and Ucayali
regions.
Results: 30 patients were interviewed. Most did not know the mechanism
of leprosy transmission. In relation to therapeutic itineraries, patients
generally went to health facilities on the recommendation of third parties who
knew the disease. In some cases, health personnel made a bad diagnosis. The
importance of the treatment indicated by the “Ministerio de Salud” (Ministry of
Health) is recognized; however, economic factors and the distance to health
facilities negatively affect adherence to treatment. In addition, it was evidenced
that stigma persists towards the disease.
Conclusions: Patients recognize the importance of treatment; however, they
express misconceptions about the pathogenesis of leprosy, and weaknesses in the
health system are also identified. These problems would lead to delay in
diagnosis and treatment. It is recommended to strengthen control strategies and
decentralize the care of leprosy with the participation of the community,
patients, health personnel and healers, considering the identified barriers and
a probable underdiagnosis in women.
Keywords: Leprosy; Health services; Perception; Therapeutics; Qualitative Research; Disability; Sociodemographic Factors; Stigma; Perú (source: MeSH NLM).
INTRODUCTION
Leprosy, considered to be a worldwide public health problem, was
reportedly eliminated as of 2000. By 2005, most countries had achieved this
goal; however, in several countries, it continues to be a problem at the regional
level (1).
The Ministry of Health (MINSA in Spanish) of Peru
reported a progressive decrease in prevalence, although there are still new
cases detected. Despite this, rates of less than 1 per 10,000 inhabitants have
been achieved in the provinces.
Most of the cases are circumscribed in the Peruvian
jungle, specifically in Loreto and Ucayali, because the disease entered these
regions through the border with Brazil in the 20th century (2). In
this context, the government policies on the control of leprosy facilitated the
introduction of anti-leprosy drugs, and achieved the control of the disease,
but not its eradication (2). In 2017, the MINSA reported eleven new
cases, including some leprosy-associated grade 2 disability, which evidences a
late diagnosis and the hidden prevalence of the disease.
|
KEY MESSAGES |
|
Motivation for the study:
In Peru, a country with a low prevalence of leprosy, patients
are still diagnosed with a leprosy associated grade 2 disability, which
suggests a late diagnosed disease.
Main findings:
Since
patients do not know the mechanism of transmission of leprosy, most of them
go to hospital following the recommendation of those who identified the
disease.
Implications:
Strategies are required to control leprosy, considering the identified
limitations of the health sector and the patients’ lack of knowledge about
the disease. |
Underdiagnosis and late diagnosis are associated
with the lack of follow-up, no active search for cases and disinformation of
people and healthcare personnel, all of which have negative consequences
influencing leprosy control (3).
Due to people’s financial problems, late diagnosis
is a result of their delay in seeking medical attention (4), and
their therapeutic itinerary (what they do and where they go to maintain or
restore their health) (5). Traditional medicine should also be
considered as influencing late diagnosis since it covers different conceptions
of health and comprises the experience and cooperation of family groups and
community (6).
The search for treatment, in contexts where different healthcare systems
coexist, is influenced by the complexity, costs and sociocultural and
geographical proximity of the health offer, which means that patients can
combine the different offers of each health system (7-9).
Leprosy control also requires knowing the
therapeutic repertoires (procedures and resources) of each healthcare system
and how patients use them (10). Likewise, adequate adherence to
treatment is required; however, it depends on socioeconomic, cultural,
psychosocial, and behavioral factors, and on adverse drug reactions (11,12).
In this context, the systems of interpretation of the disease vary within and
between cultural groups, and influence the way people prevent and treat the
disease (6,13-17).
In this concern, the objective of the study was to understand the systems of
leprosy interpretation, itineraries and therapeutic repertoires of patients
diagnosed with leprosy under treatment or after completion of treatment.
MATERIALS AND
METHODS
A qualitative study was carried out, using intentional
non-probability sampling, in which semi-structured in-depth interviews were
applied to leprosy patients under treatment or after completion of treatment.
The interviews took place between October and November 2015. Previously, the
interviewer and those responsible for the National Health Strategy for
Tuberculosis Component Lepra had a meeting with patients in order to explain in
a simple and clear way the purpose of the investigation.
The study included patients over 18 years old with
a leprosy diagnosis made in MINSA healthcare facilities, who resided at the
time of the study in the city of Iquitos (department of Loreto, province of
Maynas, districts of Belen, Punchana and San Juan Bautista) those who resided
in the city of Pucallpa (department of Ucayali, province of Coronel Portillo,
districts of Calleria, Yarinacocha and Manantay). The eight profiles
established for patients in each region included leprosy treatment (under treatment
or treatment completed), domicile (urban or rural), and sex (female or male).
The interviews were held by a healthcare
professional with experience in community work in several native communities
and qualitative study conduction, who had an induction regarding the research
topic by the team of researchers (anthropologist and infectious disease
experts in the management of leprosy patients). The interviewer also lived in
one of the included regions, which allowed an easier understanding with patients,
since he knew the mores and cultural terms used to communicate colloquially.
It is worth mentioning that all the interviews were carried out at patients’
homes, ensuring privacy and confidentiality.
Considering the theories of Chrisman (5),
Kleinman (6),
Young (7),
Schartz (8)
and Good (13), three study dimensions were proposed:
leprosy interpretation systems, therapeutic itineraries, and therapeutic
repertoires used by patients with leprosy diagnosis, including adherence to
treatment. A total of 20 codes were proposed for each dimension, based on the
objective and the study dimensions. In addition, the interview guide was
prepared and reviewed by an expert leprosy dermatologist and by a healthcare
worker with experience in community work, and modified according to their
suggestions. The final version of the guide was applied to people who
voluntarily decided to participate in the study. The interviews were carried
out until reaching the saturation point of information (30 interviews).
An inductive analysis was proposed, for which the
interviews were transcribed, and a content analysis of each one was carried
out, in Excel, finding information only on 16 of the 20 codes initially
proposed. During this analysis, an additional dimension of analysis was found:
the impact of leprosy on people’s lives, but it was not considered because it
was not the object of the study. The 16 analysis codes were validated by two
specialists on the subject (coordinator of the leprosy control program
nationwide and a dermatologist from the Regional Hospital of Iquitos). A
descriptive analysis of the sociodemographic characteristics of the study
subjects was performed, summarizing the numerical variables according to their
median and the categorical variables according to their percentage. Later,
researchers traveled to Loreto and Ucayali to triangulate the data and to get
feedback from the participants about the findings.
This study was approved by the Ethics Committee of
the National Institute of Health of Peru (INS in Spanish) through Memorandum
080-2015-CIEI-INS (Code OI-052-14). In addition, patients who agreed to
participate in the study were asked to sign the informed consent.
RESULTS
Thirty patients were included (10 of whom were women) —10 from
rural areas and 20 had completed their treatment. Most of the patients who had
completed the treatment were over 50 years old and received their first
treatment at the San Pablo leprosarium (Table 1).
Table 1. Sociodemographic characteristics of patients
included in the study.
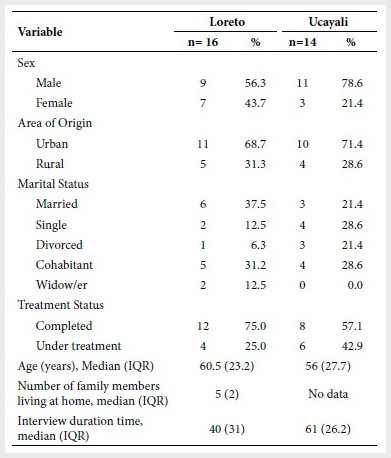
IQR: interquartile range
Interviews were conducted for the following
profiles: under treatment urban man (7 patients), under treatment urban woman
(1 patient), under treatment rural man (2 patients), urban man with treatment
profile (7 patients), urban women with treatment profile (5 patients), rural
man with treatment profile (4 patients) and rural woman with treatment profile
(4 patients). The analysis by dimensions is presented, considering the codes of
the most relevant findings. The complete analysis is attached as a supplementary
material: annex 1, 2 and 3.
Interpretation
systems on leprosy
Regardless of patient’s sex, age and area of origin, various responses were identified regarding the form of leprosy transmission, i. e., presence of a strange person or a sick person at home, washing a sick person’s clothes or shaking hands with them, sexual contact with a sick person, leaving their communities, exposure to polluting agents, such as sewage or forest diseases, or the intake of certain foods (such as the Amazonian tapir or the armadillo), “divine will”, and hereditary factors.
“Maybe my ancestors had it. You know the genetic
order, it never disappears, it follows its rhythm maybe your children don’t get
it, but your great-grandchildren may…”
55-year-old urban man from Ucayali, under
treatment.
Another perception was that the microorganisms
causing leprosy or other diseases are with the person since they are born and
it develops depending on their immune response.
Transmission by air was also mentioned by three
patients who reported that leprosy spreads when talking to an infected person;
however, they do not show security in this response, since they later justify
their contagion by other ways. It was also possible to identify that the
perception that leprosy is a highly contagious disease still present
(46-year-old rural man); while other interviewees reported that it was not
contagious (76-year-old rural woman and 78-year-old urban woman).
Regardless their area of origin and sex, patients
aged between 70 and 79 years old reported four ways to prevent spreading the
disease —not having sex with an infected person, sleeping separately, not
kissing on the mouth, burning mattresses and sheets after healing, have
separate personal supplies and eat well.
“Did you say ‘I should sleep apart’, or your wife
told you to do so? I said it should be better if I
sleep apart because maybe she can catch it from me ...”
41-year-old urban man from Ucayali, under
treatment.
Regarding the consequences of abandoning treatment,
the responses comprised relapses, death, disability and death from complications.
This speech was held by all patients regardless of their area of origin, sex
and age.
“If you stop the treatment, it can happen again, (...) maybe you
don’t take medication, you
might get sick again, death can
happen too”.
71-year-old rural woman from
Loreto, cured.
Usually the discourse used is that leprosy, following
polychemotherapy, is curable; however, an 81-year-old rural patient mentioned
that it was incurable since the disease is permanently in the blood. On the other
hand, it is recognized by patients that before there was no treatment for leprosy
and that patients died.
“Well, he told me that this disease can be cured,
it is not incurable. There is a cure, many people (...) I have talked with the
doctor then he indicated to me what it is that I must do”
58-year-old urban man from Loreto, under treatment.
Therapeutic
itineraries in leprosy
Regardless of sex and age, the patients stressed that family
support (especially from the wife) is important for them to go to a health
facility and comply with the treatment and controls. However, a 71-year-old
woman from the rural area stated that her relatives turned their backs on her
for fear of contagion. Another patient stated that his teacher identified the
spots and took him to the hospital for diagnosis.
A misdiagnosis due to the lack of experience of
health personnel can cause the patient to lose confidence and seek other
treatment options, which may lead to delayed diagnosis. This finding was
identified in two young urban patients under the age of 35.
Three patients under 50 years old (two from rural
areas and one from urban areas) with treatment completed reported having
consulted a local non-medical healer (curandero/witchdoctor) when they did not
find improvement in symptoms. A 26-year-old male patient from the urban area
mentioned that the local non-medical healer referred him to the hospital. He
stated that he did not believe in witchdoctors, but that he was taken to one by
his sisters.
“Did you go to the medicine man? Yes,
of those who cure witchcraft (...) I went because my sisters recommended me
when they saw that I had not improved. I went after the treatment, I thought
that once treatment is completed, then leprosy was over, but not really, it
takes time to disappear from your body.”
26-year-old
urban man from Ucayali, under treatment.
Regardless of the area of origin and sex, patients
think that healthcare for leprosy is limited, with difficult geographical
access and that there is a lack of specialists. Those are their barriers
against an early diagnosis and treatment.
The hospital and leprosy program were identified as
the place where the disease is primarily treated. The patients also pointed out
other places of care, such as Hospital de la Solidaridad, in Lima, the
Institute of Tropical Medicine of Universidad Nacional Mayor de San Marcos and
private clinics. Interviewees over 70 years old who completed their treatment
identified the leprosarium of San Pablo as the place of care. Pharmacies were
not recognized as options either.
“Hives have appeared (...) most people talked, and
since in Pucallpa there were also infected people who came by raft, back in
Contamana, they picked me up and took me to San Pablo.”
67-year-old rural woman from Loreto, cured.
Likewise, half of the interviewees identified a
certain MINSA doctor or technician as the person makes the diagnosis or
provides treatment (a single doctor or technician was identified for each of
the patient’s cities).
Therapeutic
repertoire of leprosy and adherence to treatment
In
relation to the treatments used, the patients indicated that they took
different types of drugs over the years, and in addition, they used vegetables,
mud and medicinal plants, such as ayahuasca, chirimasango with sacha garlic,
catahua, marco sacha, bark of cedar, etc. Treatments given by relatives or non-medical
healers.
“... and at that time my father was still living
and said to me: ‘I am going to bring you a remedy
that
is effective,’ and he brought me a jungle root named male sacha ajoma (...),
and then chirisamango. I drank a liter
of it, and that numbness disappeared for like ten years”
58-year-old urban man from Loreto, under treatment.
Patients highlighted the importance of starting
treatment early as a measure to avoid contagion or complications, but it was
also evidenced that patients have the perception that, despite having completed
treatment, leprosy could be within them and that it could manifest again.
External factors that negatively affect adherence
to treatment: living far from health centers, limited hours of attention from
health centers and limited financial resources, especially in rural patients.
Side reactions (especially gastrointestinal), patient’s lifestyle (drinking and
smoking) and presence of other diseases, such as knee joint problems, were also
mentioned, as they stated that they could not take as much medicine at the same
time (70-year-old urban man).
“No, I did not leave because I practically lived
here, I did not have the resources to go to Atalaya, to Pucallpa...”
49-year-old rural man from Ucayali, under
treatment.
Approximately half of the patients, state that they
have Health Insurance (SIS in Spanish), support from doctors and transfers to
health facilities near their town to receive treatment. Regardless of sex, area
of origin and age, it was identified that the accompaniment of the family,
especially wife and children, favors adherence. It was not possible to identify
that friends or neighbors fulfilled this role.
Regardless of patients’ area of origin, sex and
age, they reported to have avoided eating red meat, or high-fat foods, some
fish, chili or drinking beer during treatment in order not to increase liver or
kidney disorders associated with treatment. They also avoided eating fish with
bones or pork because they associate it with the appearance of lepromatous lesions.
“When you were under treatment what things did you
not eat? When I started to swallow the pills every day, I ate everything, I
just didn’t drink beer, I didn’t smoke, I didn’t eat pig, chili
...”
46-year-old rural man, with treatment completed.
DISCUSION
Most of the patients who were receiving or had received
treatment in a MINSA health facility were unaware of the way in which leprosy
spread. Although most of them associated it with a form of contagion, only
three patients mentioned airborne contagion. This could be explained by the
social representation of the disease, associated with perceptions of
incurability and contagiousness, which in turn is related to the stigma
associated with physical deformities (14,15). Most of the interviewed patients had completed
treatment, and many had sequelae, due to late initiation of treatment, or
because they contracted the disease many years ago when there was no specific
treatment, which may explain the perceptions of incurability associated with
lack of understanding and knowledge about the disease (15,16).
Despite the fact that, in our study, the interviewees stated that they were
cured thanks to polychemotherapy and recognized the consequences of abandoning
treatment, this “cured” condition from the perception of the affected person
and the community is “misleading”, because some patients continue to feel
infected, both among those with or without disabilities (15).
The study showed that the majority of the patients went to the
hospitals or smaller medical centers on the recommendation of others. The
influence of close family members in seeking help for the diagnosis of the
disease was very important. The literature indicates that the influence of
social networks motivates patients to seek the definitive diagnosis; otherwise,
the affected will not do it by themselves. This behavior could respond two
reasons: despite having previous experience with the disease, these patients
were not aware of the risk to which they were exposed, or despite suspecting
that they have leprosy, they were silent for fear of social rejection; for
these reasons, decision-making about whether or not to go to a health center
would also be influenced by accumulated negative social experiences (18,19).
In relation to the therapeutic itinerary, we found
that the quality of health services, especially, first level and private
clinics, was inefficient. In some of the cases they gave a bad diagnosis,
delaying the start of treatment; this finding agrees with Naaz, et al. where it is reported that local professionals have poor
knowledge about leprosy, although this study describes little referral to
specialized centers (15). These researchers have indicated that patients who go
to the most complex hospitals are 6.6 times more likely to receive timely treatment
(15).
However, for our reality, and in the search of the eradication of leprosy, it
is necessary to strengthen first-level health care facilities to capture
probable cases of leprosy, through dermatological screening and home contacts (20).
It is important to highlight that the majority of
patients report that health services are limited, that there are few
specialists, and in several cases, there is difficulty in accessing health
facilities, either due to the remoteness of these, or for the economic cost of
the transfer. This constitutes barriers to early diagnosis and treatment, and
make therapeutic adherence difficult.
In addition, the need to strengthen knowledge about
the disease in patients, the community and healthcare personnel has been evidenced,
lack of knowledge is associated with delay in seeking medical care and failure
to treatment adherence (21, 22). In this sense, only two patients
indicated that the initiation of treatment is very important to avoid
disability, despite the fact that the relationship between disability,
treatment and timely diagnosis is supported by various studies (15,23).
The delay in diagnosis is related to ignorance of the disease by health
personnel, therefore, it is important to reinforce education on this pathology
in professionals in the provinces with cases of leprosy (21,22).
Regarding the search for care by non-medical
healers, approximately a third sought care with non-medical healers, including
patients under treatment. This has been described in other studies, where it
was found that the majority of the study participants received the first
treatment from witchdoctors and traditional healers (18).
Currently, it has been shown that non-medical healers are trusted (although in
a limited way), creating the need to incorporate said healer as “a complementary
medical support” within the biomedical system (24), possibly to fulfill roles
of referral mediators between patients and hospitals.
Peru has a low prevalence of leprosy; therefore,
the detection of new cases should be accompanied by a strict follow-up of
contacts, social participation of those affected and the community, and in
addition to trained professionals and surveillance centers for drug resistance (20,25).
However, in our study and other previous studies, two major problems have been
evidenced: the lack of experience of healthcare personnel in detecting the
disease (15)
and disjointed work between health centers, the community, and a
specialized hospital, to control leprosy. Likewise, other studies have
described that stigma and discrimination are negative psychosocial factors
that play an important role in the elimination of leprosy; therefore, public
policies should be aimed at establishing measures that address these issues (20,25).
Among the limitations of the study, the difficulty
of obtaining at least two interviews for each profile stands out. This is
related to the decrease of new cases of leprosy in the country, and that the
new cases are scattered in remote districts. Likewise, it was observed that
there was greater difficulty in encountering female patients undergoing
treatment in both rural and urban areas, and this could limit our results
regarding their perceptions of leprosy; however, this could be explained by the
epidemiology of leprosy in the country, where according to national reports,
new cases are mostly in men. Despite the fact that the diagnosis of leprosy has
been reported to be more frequent in men than in women, this differs
statistically from other countries such as Brazil, where leprosy cases in Mato
Grosso are more frequent in women, which should be evaluated with caution due
to the possible underdiagnosis of leprosy in women (26,27).
Another important limitation of the study was that
the person who conducted the interviews did not participate in the design of
the project or in the analysis of the interviews. Despite the limitations, we
believe that the results are relevant, since similar studies have not been
conducted in Peru. These results can help strengthen leprosy elimination
strategies at the district level, considering those cities with new cases in
recent years.
In conclusion, patients recognize the importance of
leprosy treatment, however, they express misconceptions about the pathogenesis
of this disease and weaknesses in the health system are identified. These
problems would lead to delayed diagnosis and treatment of the disease. It is
recommended to strengthen control strategies and decentralize leprosy care with
the participation of the community, patients, healthcare personnel and
non-medical healers, considering the identified barriers and a probable
underdiagnosis in women. This will influence the eradication of leprosy in the
country.
Acknowledgments:
To Mg. Efraín Ayala Remón, for his support in conducting the interviews and transcription and the anthropologist Enzo Morales for his support in the analysis of the information.
REFERENCES
1. World
Health Organitation. Weekly epidemiological record
[Internet]. WHO. 2016 [citado el 4 de diciembre del 2019]. Disponible en: https://www.who.int/wer/2016/wer9135.pdf.
2. Burstein
Z. Revisión histórica del control de la Lepra en el Perú. Rev
perú med exp salud pública [Internet]. 2001 [citado el 28 de
diciembre del 2019]; 18(1-2):40-4. Disponible en: http://www.scielo.org.pe/scielo.php?script=sci_arttext&pid=S1726-46342001000100010&lng=es.
3. Acosta J. Evaluabilidad del Programa de eliminación de la lepra en el
Perú [tesis de master]. Granada: Escuela Andaluza de Salud Pública, Universidad
de Granada; 2013.
4. Peters
RMH, Dadun, Lusli M,
Miranda-Galarza B, Van Brakel WH, Zweekhorst
MBM, et al. The meaning
of leprosy and everyday experiences: an exploration in cirebon,
indonesia. J Trop Med
[Internet]. 2013 [citado el 30 de diciembre del 2019]; 2013: 507034. Disponible
en: https://doi.org/10.1155/2013/507034.
5. Chrisman
NJ. The health seeking process: an approach to the natural history of illness. Cult Med
Psychiatry [Internet]. 1977 [citado el 14 de
diciembre del 2019];1(4):351-77. Disponible en: https://doi.org/10.1007/BF00116243.
6. Kleinman
A. Concepts and a model for the comparison
of medical systems as cultural systems.
Soc Sci Med
[Internet]. 1978 [citado el 10 de diciembre del 2019]; 12(2B):85-93. Disponible
en: https://doi.org/10.1016/0160-7987(78)90014-5.
7. Young A. The anthropologies of illness and sickness. Annu Rev Anthropol
[Internet]. 1982 [citado el 20 de diciembre del 2019]; 11:257-85. Disponible
en: https://doi.org/10.1146/annurev.an.11.100182.001353
8. Schwartz
LR. The hierarchy of resort in curative practices: The Admiralty
Islands, Melanesia. J Health Soc Behav [Internet]. 1969 [citado el 14 de diciembre
del 2019];10(3):201-9. Disponible en: https://doi.org/10.2307/2948390.
9. Simionato
I, Moraes M, Viera A, Seles L, Samboni
T, Arrollo L, et al. Social determinants, their relationship with leprosy risk
and temporal trends in a triborder
region in Latin America. PLoS Negl
Trop Dis [Internet]. 2018
[citado el 7 de diciembre del 2019]; 12(4): e0006407. Disponible en: https://doi.org/10.1371/journal.pntd.0006407.
10. Chamorro A, Tocornal C. Prácticas de salud en las comunidades del Salar
de Atacama: Hacia una etnografía médica contemporánea. Estud
Atacam [Internet]. 2005 [citado el 10 de diciembre
del 2019];(30):117-34. Disponible en: http://dx.doi.org/10.4067/S0718-10432005000200007.
11. Honrado ER, Tallo V, Balis AC, Chan GP, Cho SN. Noncompliance with the world health
organization-multidrug therapy
among leprosy patients in Cebu, Philippines: its causes and implications on the leprosy control program. Dermatol Clin [Internet]. 2008 [citado el 17 de enero del 2020]; 26
(2): 221-9. Disponible en: https://doi.org/10.1016/j.det.2007.11.007.
12. Heukelbach
J, Chichava OA, Rodriguez
de Oliveira A, Häfner K, Walther
F, Morais de Alencar CH, et
al. Interruption and Defaulting
of Multidrug Therapy against Leprosy: Population-Based Study in Brazil’s Savannah Region. PLoS Negl Trop
Dis [Internet]. 2011 [citado el 30 de diciembre del
2019]; 5(5): e1031. Disponible en: https://doi.org/10.1371/journal.pntd.0001031.
13. Good
BJ. Medicina, racionalidad y experiencia: una perspectiva antropológica.
Barcelona: Bellaterra Ediciones Barcelona; 2003.
14. Van
Brakel WH , Sihombing
B, Djarir
H, Beise
K ,
Kusumawardhani L , Yulihane R, et
al. Disability in people
affected by leprosy: the role of impairment, activity, social participation, stigma and discrimination. Glob
Acción para la Salud [Internet]. 2012 [citado el 10 de
diciembre del 2019]; 5:10. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3402069.
15. Naaz
F, Mohanty PS, Bansal AK, Kumar D, Gupta UD. Challenges Beyond Elimination in Leprosy. Int J
Mycobacteriol [Internet]. 2017 [citado el 10
de diciembre del 2019]; 6(3):222-8. Disponible en: http://www.ijmyco.org/text.asp?2017/6/3/222/211929.
16. Sermrittirong
S, Van Brakel W, Kraipui N,
Traithip S, Bunders-Aelen
J. Comparing the perception of community members towards leprosy and tuberculosis stigmatization.
Lepr Rev. 2015; 86(1): 54–61.
17. Valsa A, Longmore M, Ebenezer M, Richard
J. Effectiveness of Social Skills
Training for reduction of self-perceived Stigma in Leprosy Patients in rural India -
a preliminary study. Lepr Rev. 2012; 83(1): 80- 92.
18. Adhikari
B, Kaehler N, Chapman RS, Raut
S, Roche P. Factors Affecting
Perceived Stigma in Leprosy Affected Persons in Western Nepal. PLoS
Negl Trop Dis
[Internet]. 2014 [citado el 7 de diciembre del 2019]; 8(6): e2940. Disponible
en: https://doi.org/10.1371/journal.pntd.0002940.
19. Susanti
IA, Mahardita
NGP, Alfianto
R , Sujana IMIWC , Siswoyo , Susanto T. Social stigma, adherence to medication
and motivation for healing: A cross-sectional study of leprosy patients at Jember Public Health
Center, Indonesia. J Taibah Univ
Med Sci [Internet]. 2017
[citado el 5 de diciembre del 2019]; 13 (1): 97-102. Disponible en: https://doi.org/10.1016/j.jtumed.2017.06.006.
20. Li J, Yang L, Wang Y, Liu H, Cross H. How to improve early case detection in low endemic areas with
pockets of leprosy: a study of newly detected leprosy patients in Guizhou Province, People’s Republic of China. Lepr Rev. 2016; 87(1): 23-31.
21. Martins
RJ, Oliveira ME, Saliba SA, Saliba
SA, Ísper AJ. Sociodemographic
and epidemiological profile
of leprosy patients in an endemic region
in Brazil. Rev Soc Bras Med
Trop [Internet]. 2016 [citado el 5 de enero del
2020]; 49(6):777-780. Disponible en: http://dx.doi.org/10.1590/0037-8682-0069-2016.
22. Lira
KB, Leite
JJ, Maia DC, Freitas R , Feijão AR. Knowledge of the patients
regarding leprosy and adherence to treatment. Braz J Infect Dis [Internet]. 2012 [citado el 11 de enero del 2020];
16(5):472-5. Disponible en: http://dx.doi.org/10.1016/j.bjid.2012.04.002.
23. Matos
AMF, Coelho
ACO ,
Araújo LPT, Alves MJM, Baquero OS, Duthie MS, et al. Assessing epidemiology of leprosy and socio-economic distribution of cases. Epidemiol
Infect [Internet]. 2018 [citado el 7 de diciembre del 2019];
146(14): 1750-55. Disponible en: https://doi.org/10.1017/S0950268818001814.
24. Eysaguirre
CF. El proceso de incorporación de la medicina tradicional y alternativa y
complementaria en las políticas oficiales de salud [tesis de máster]. Lima:
Facultad de ciencias sociales, Universidad Mayor de San Marcos; 2016.
Disponible en: http://cybertesis.unmsm.edu.pe/handle/cybertesis/6274.
25. Cairns
W, Smith S. Leprosy: making
good progress but hidden challenges
remain. Indian J Med Res [Internet]. 2013 [citado el 11 de enero del 2020];
137:1-3. Disponible en: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3657869/.
26. Zhang F, Chen S, Sun Y, Chu T. Healthcare seeking behaviour and delay in diagnosis of leprosy in
a low endemic area of China. Lepr Rev [Internet]. 2009 [citado el 11 de enero del 2020];
80(4):416-23. Disponible en: https://www.lepra.org.uk/platforms/lepra/files/lr/Dec09/Lep416-423.pdf.
27. Walker SL, Withington SG, Lockwood DNJ. Leprosy. En: Farra J, Hotez P, Junghanss T, Kang G, Lalloo, White N, editores. Manson’s
Tropical Infectious Diseases
[Internet]. 23a ed. 2014 [citado el
12 de enero del 2020]. p 506-18 Disponible en: https://www.elsevier.com/books/mansons-tropical-infectious-diseases/9780702051012-
Funding:
The research was funded by the 2014 Competitive Fund of the National Center for
Public Health of the National Institute of Health of Peru.
Supplementary
material:
Available in the electronic version of the PSRP
Citation:
Osorio-Mejía C, Falconí-Rosadio E, Acosta J. Interpretation
systems, therapeutic itineraries and repertoires of leprosy patients in a low
prevalence country. Rev Peru Med Exp Salud Publica.
2020;37(1):25-31. Doi:
https://doi.org/10.17843/rpmesp.2020.371.4820
Correspondence to:
Carmen Edith Osorio Mejía; Av. Defensores del Morro 2268, Chorrillos.
Lima, Perú;
caome22@gmail.com
Authorship contributions: JA and
EFR have participated in the conception and design of the study. JA and COM
participated in the collection, analysis of data and writing of the article. In
addition, JA participated in the obtention of funding. All three authors
approved the final version of the article.
Conflicts of interest:
The authors declare to have no
conflicts of interest in relation to this publication.
Received:
20/09/2019
Approved:
22/01/2020
Online:
19/03/2020