BRIEF REPORT
Cost variability of antipsychotics according to pharmaceutical
establishments in Lima, Peru
Rubén
Valle ![]() 1,2
, Psychiatrist,
Master of Science in Epidemiological Research
1,2
, Psychiatrist,
Master of Science in Epidemiological Research
1
Centro de Investigación en Epidemiología
Clínica y Medicina Basada en Evidencias, Facultad de Medicina Humana,Universidad
de San Martín de Porres, Lima, Peru.
2 DEIDAE de Adultos y Adultos Mayores,
Instituto Nacional de Salud Mental «Honorio Delgado - Hideyo Noguchi», Lima,
Peru.
ABSTRACT
The
objectives of the study were to determine the cost variability of
antipsychotics in public (hospitals) and private pharmaceutical establishments
(pharmacies and clinics), calculate the cost variability of antipsychotics
between establishments and estimate the cost of monthly maintenance treatment
with antipsychotics. A cost analysis study was performed, unit costs of
antipsychotics were obtained from the Peruvian Pharmaceutical Products
Observatory. The results show that the cost variability of antipsychotics was
greater in pharmacies and clinics than in hospitals, and the analysis of cost
variability between pharmaceutical establishments showed that the cost of an
antipsychotic in a pharmacy and clinic was 1.3 to 140 times and 2.8 to 124
times, respectively, the cost of the drug in a hospital. The cost of monthly
maintenance treatment varied from S/ 3 to S/ 2130 according to the drug and
pharmaceutical establishment.
Keywords: Costs and Cost analysis; Antipsychotic Agents; Schizophrenia; Mental Disorders; Peru (source: MeSH NLM).
INTRODUCTION
Antipsychotics are a group of drugs used in the
treatment of various mental disorders. These drugs are considered the cornerstone
of treatment for psychotic disorders (1). Some of these have been
approved for the treatment of bipolar disorder (2), or are used in an
unapproved way in the obsessive-compulsive disorder and personality disorder (3,4).
Antipsychotics are effective in reducing the symptoms of psychosis and differ
in the profile of side effects they can produce (5). These drugs should
be taken daily (oral) or periodically (deposit) to avoid relapses and to help
in the recovery process (6,7). It is therefore
important that health systems can ensure access to these drugs.
Patients
recibing antipsychotics, who are users of the Integral Health Insurance (SIS),
receive the drugs free of charge in the Ministry of Health (MINSA) facilities.
However, access to these drugs in MINSA institutions is limited since only 78%
of the institutes, 64% of the hospitals, 8% of the centers, and 1% of the
medical posts have antipsychotics (8). This situation leads
patients to buy their medicines in private pharmacies at a higher cost, with
the consequent increase in out-of-pocket expenses (8). Relapses can also
occur because of reducing the dose or even discontinuing treatment because
patients cannot afford it. Clinical relapses, in turn, lead to higher expenses
for the health system due to the use of more expensive services such as
emergency or hospitalization (9).
The
costs of antipsychotics vary widely in the marketplace. The cost variability
(ratio of lowest to highest cost) of risperidone in India is 1 to 16, and
olanzapine 1 to 12; the variability of these drugs in Brazil is 1 to 35,000 and
1 to 79, respectively (10,11). Antipsychotics can have high costs,
which results in less access to these drugs and the possibility that patients
may not be able to continue treatment. In Peru, one report showed wide
variations in the cost of drugs, with the cost of a drug being ten times higher
in a private pharmacy than in a public one (12). However, the variability of
antipsychotic costs has not been specifically studied.
|
KEY MESSSAGES |
|
Motivation for the study:
Although antipsychotics are useful for the
management of several mental disorders and must be taken for a long time,
these can be expensive, making access to these medicines difficult.
Main findings:
The unit cost and monthly treatment with antipsychotics is
higher in pharmacies and clinics than in hospitals. The cost of monthly
treatment varies from S/3 to S/2,130 depending on the drug and pharmaceutical
establishment.
Implications:
Public hospitals must ensure that they have enough
antipsychotics supply so that users of these drugs do not have problems in
obtaining them. |
The
objectives of the study are to determine the variability of antipsychotic costs
in public (hospitals) and private (pharmacies and clinics) pharmaceutical
establishments, to estimate the variability of antipsychotic costs between
pharmaceutical establishments and to estimate the cost of monthly treatment
maintenance with antipsychotics in monotherapy.
THE STUDY
This is a cost analysis partial economic study
according to the user’s perspective. The unit costs of antipsychotics were
obtained from the Peruvian Observatory of Pharmaceutical Products (OPPF) of the
General Directorate of Medicines, Supplies and Drugs (DIGEMID), where
pharmaceutical establishments post information on the costs of drugs (13).
Peru’s Single National Request for Essential Medicines contains the generic
names of the antipsychotics entered into the search engine, other antipsychotics
used in psychiatric care were also included (14). The search provided information
on the pharmaceutical establishment, date of data update, product name,
laboratory name, unit cost, and technical information of the product.
Public
pharmaceutical establishments in MINSA and DIGEMID hospitals were categorized
as “hospitals”; pharmaceutical establishments like apothecaries and private
pharmacies were categorized as “pharmacies”; and pharmaceutical establishments
such as private clinics were categorized as “clinics”. In addition,
antipsychotics whose name corresponded to the International Non-proprietary
Names for Pharmaceutical Substances (INN) were categorized as “generics”; those
whose name corresponded to the drug studied in a pharmacological research and
which obtained the patent were categorized as “innovative drugs”; and antipsychotics
which were listed under a trade name, but different from that of the innovative
drugs, were categorized as “branded generics” (15).
The
descriptive analysis consisted of calculating the median, minimum and maximum
value of the cost of the antipsychotic according to the type of drug and
pharmaceutical establishment. The cost variability analysis by antipsychotic
compared the minimum and maximum cost of an antipsychotic of the same
formulation dispensed by the same type of pharmaceutical establishment. The
analysis of cost variability between pharmaceutical facilities compared the
median cost of an antipsychotic in a hospital with that of a pharmacy and a
clinic. The estimate of the cost of monthly maintenance treatment with
antipsychotics in monotherapy was made based on the upper limit of the
maintenance dose range of each antipsychotic according to the international
consensus study on dosage (16). The analysis was performed with the
statistical program Stata v12 (StataCorp LP, College Station, TX, USA).
RESULTS
Data on 11 antipsychotics was available from the OPPF
as of July 5th, 2019: six of first-generation and five of second-generation.
Data had been entered at the OPPF between May 5th and July 4th, 2019. Only
three antipsychotics were available as innovative drugs: haloperidol decanoate
(Haldol decanoes), quetiapine (Seroquel) and olanzapine (Zyprexa). The data
were reported mostly by pharmacies (77.4%-99.9%), followed by hospitals
(0.1%-100%) and clinics (0.1%-6.5%) (Table 1).
Table 1:
Availability
of antipsychotics by pharmaceutical establishment and type of drug in Lima
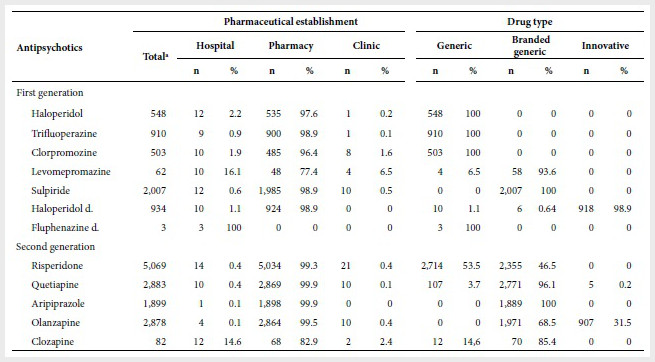
a
Establishments that supply antipsychotics according to the Peruvian Observatory
of Pharmaceutical Products. d: decanoate.
Antipsychotic costs
The median of the unit costs of oral antipsychotics
was lower in hospitals than in pharmacies and clinics. Median costs of antipsychotics
in hospitals ranged from S/ 0.1 (haloperidol) to S/ 1.3 (aripiprazole), in
pharmacies from S/0.68 (chlorpromazine) to S/ 24.0 (olanzapine) and in clinics
from S/ 0.5 (haloperidol) to S/ 38.9 (olanzapine). The median costs of generic
antipsychotics were lower than branded generic ones (except for risperidone
sold in hospitals), and their costs were lower than those of the innovative
drugs. This trend was also observed for haloperidol decanoate. Fluphenazine
decanoate was only available in hospitals at a (median) cost of S/ 9.5 (Table 2).
Table 2.
Unit cost of antipsychotics according to pharmaceutical establishment and type
of drug in Lima
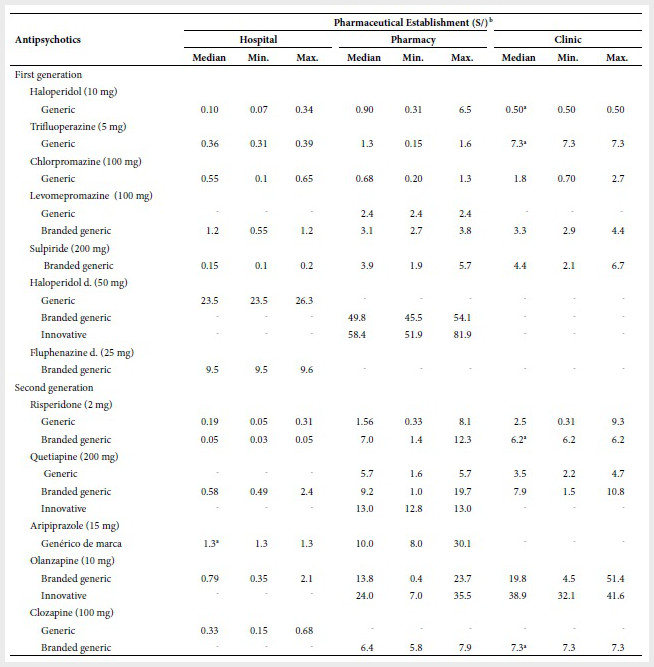
a
There was only one observation; b costs less than S/1 are
represented with two decimals.
d:
decanoate; Min.: minimum; Max.: maximum; hyphen (-): no data was reported.
Cost variability by antipsychotic, and between
pharmaceutical establishments
The greatest variability in hospital costs was 1 to
6.5 for generics (chlorpromazine) and 1 to 6 (olanzapine) for brand generics.
In pharmacies, the greatest variability in generics was 1 to 24.5
(risperidone), in branded generics was 1 to 59 (olanzapine) and in innovative
drugs was 1 to 1.6 (haloperidol decanoate). In clinics, the highest variability
in generics was 1 to 30 (risperidone), in branded generics was 1 to 11
(olanzapine) and in innovative drugs was 1 to 5.1 (olanzapine).
The
greatest variability in costs between hospitals and pharmacies was described
for haloperidol (1 to 9) and in branded generics for risperidone (1 to 140).
Between hospitals and clinics, the highest cost variability regarding generics,
was for trifluoperazine (1 to 20.3) and in branded generics was for risperidone
(1 to 124) (Table 3).
Table 3.
Cost
variability by antipsychotic and among pharmaceutical facilities in Lima
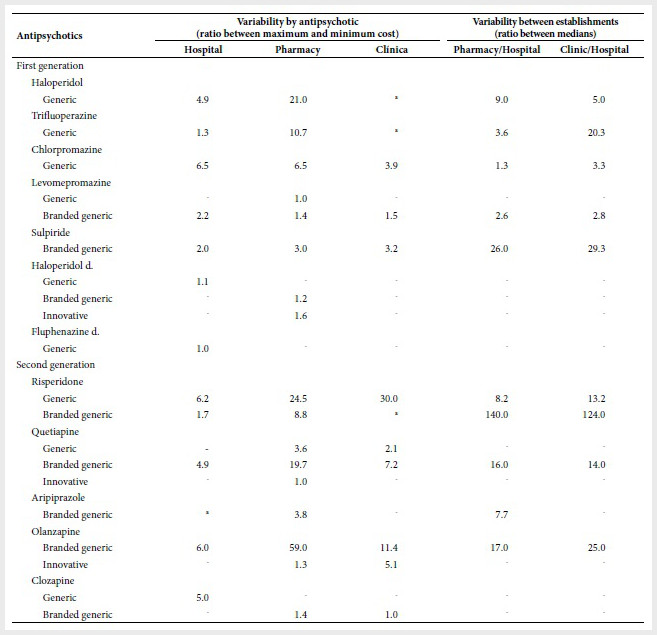
a
There was only one observation.
d:
decanoate, Min.: minimum, Max.: maximum; hyphen (-): no data was reported.
Cost of monthly treatment
The maintenance cost of monthly treatment with
antipsychotics was lower in hospitals than in pharmacies and clinics. The
monthly treatment cost varied from S/ 3 (generic/ haloperidol) to S/ 144
(levomepromazine/branded generic) in hospitals, from S/ 27 (haloperidol/generic)
to S/ 1,560 (olanzapine/innovative) in pharmacies from S/ 15
(haloperidol/generic) to S/ 2,130 (olanzapine/innovative) in clinics. Treatment
cost in pharmacies and clinics with generic, risperidone, quetiapine and
levomepromazine (pharmacies only) was higher than with their branded generics
in hospitals. The cost of monthly treatment in hospitals with haloperidol
decanoate (S/ 70.5) was almost double that of fluphenazine decanoate (S/ 38)
(Table 4).
Table 4.
Estimate
of monthly cost of maintenance treatment with antipsychotics
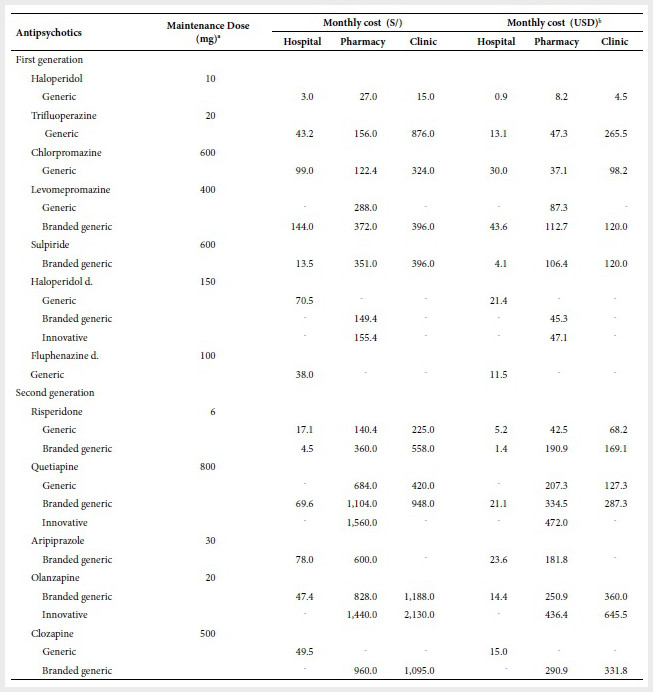
a
Based on the international consensus study on antipsychotic dosage (16).
The doses are not necessarily comparable. b
Exchange rate: 1 USD= S/3.3.
d:
decanoate; hyphen (-): no data was reported.
DISCUSSION
The study provides an economic perspective on the
cost of antipsychotics and the treatment cost of these drugs. The results show
that the cost variation is greater in private pharmaceutical establishments
(pharmacies and clinics) rather than in public establishments (hospitals). The
selling price of a drug in this sector cannot exceed 25% of its purchase price (17) this could be the cause for the small
variability of antipsychotic costs in hospitals. While the high variability of
costs in pharmacies and clinics could be due to the lack of regulation in the
antipsychotic drug costs (18). Thus, the different type of regulation
between the public and private sectors would explain the differences in the
variability of the costs of antipsychotics.
It
has been argued that the higher cost in private establishments is because these
centers sell “brand” medicines with a purchase cost higher than that of the
generic ones (12), and because the public sector makes corporate
purchases that allow the public sector to sell medicines at a low cost. In
contrast, our study shows that some generic branded antipsychotics in hospitals
cost less than their generic counterparts sold in pharmacies and clinics. In
addition, private pharmacies in Peru have had a merger process that allows them
to manage a large part of the market and therefore make corporate purchases (18). In
this sense, the high cost of antipsychotics in pharmacies and clinics seems to
be exclusively due to market laws and the search for higher profit margins.
The
estimate of the cost of monthly maintenance treatment was made based on a
monotherapy scheme when polypharmacy, the joint use of more than one
psychotropic drug, is more common (19). Polypharmacy is not
supported by evidence and adds higher treatment costs by adding an
antipsychotic or other psychiatric drug to the therapeutic scheme; however, it
is widely used in our setting. For example, two studies in patients with
schizophrenia showed that 40.5% of outpatients and 57% of inpatients received
more than one antipsychotic (20,21). Therefore, the treatment costs in
our study only apply to monotherapy treatment and not to polypharmacy
treatments whose cost would be higher.
The
study has some limitations. A report from the Ombudsman’s Office found that the
coincidence between the cost of medicines in pharmacies and the OPPF was 69.3%
(12),
so it is likely that a percentage of the costs of antipsychotics from the OPPF
may be different from the costs they have in pharmacies due to a lack of an
update or under-reporting by pharmacies. The estimate of the cost of monthly
maintenance treatment was made on the basis of recommended doses and not the
prescribed doses, so our estimates may differ from the actual cost of
treatment. The inference of our results could be affected if establishments
selling antipsychotics do not report them to the OPPF; however, this
probability is low since only 6.2% of pharmacies are not registered in the OPPF
(12).
On the other hand, the data from the OPPF allowed to overcome problems of reluctance
on the part of pharmacies to provide information on the costs of medicines (22),
and allowed to know the cost of antipsychotics from a large number of
pharmacies that otherwise would have taken high resources.
In conclusion, the results show that the cost variability of antipsychotics is greater in pharmacies and clinics than in hospitals, and the analysis of cost variability between pharmaceutical establishments shows that the cost of an antipsychotic in a pharmacy and clinic can be as much as 1.3 to 140 times and 2.8 to 124 times the cost of the drug in a hospital, respectively. The cost of monthly treatment with antipsychotics in monotherapy varies from S/ 3 to S/ 2,130 depending on the type of drug and pharmaceutical establishment. The wide variability of antipsychotic costs identified in our study demands that some me-asures should be taken. The mental health authorities must ensure the supply of antipsychotics in MINSA institutions so that the SIS-affiliated population using these drugs can always receive them, and that users not affiliated to the SIS can buy them at these centers. In addition, health authorities should consider regulating the cost of antipsychotics in the private market, as is the case in other countries. Finally, physicians who prescribe antipsychotics should know the costs of these drugs, assess the cost of antipsychotics before prescribing them and comply with the technical standard of prescribing generic drugs.
REFERENCES
1. Kreyenbuhl
J, Buchanan RW, Dickerson FB, Dixon LB, Schizophrenia Patient Outcomes Research Team (PORT). The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull. 2010;36(1):94–103.
doi: 10.1093/schbul/sbp130.
2. Frye
MA. Clinical practice.
Bipolar disorder--a focus on depression. N Engl J Med. 2011;364(1):51–9. doi:
10.1056/NEJMc1101370.
3. Zhou
D-D, Zhou X-X, Lv Z, Chen X-R, Wang W, Wang G-M, et al. Comparative
efficacy and tolerability
of antipsychotics as augmentations
in adults with treatment-resistant obsessive-compulsive
disorder: A network meta-analysis. J Psychiatr Res. 2019;111:51–8. doi:
10.1016/j.jpsychires.2019.01.014.
4. Stoffers
J, Völlm BA, Rücker G, Timmer A, Huband N, Lieb K. Pharmacological interventions for borderline personality disorder. Cochrane Database Syst Rev. 2010;(6):1–166. doi: 10.1002/14651858.CD005653.pub2.
5. Leucht
S, Heres S, Kissling W, Davis JM. Evidence-based
pharmacotherapy of schizophrenia.
Int J Neuropsychopharmacol.
2011;14(2):269–84. doi: 10.1017/S1461145710001380.
6. Kishi
T, Ikuta T, Matsui Y, Inada K, Matsuda Y, Mishima K, et al. Effect of discontinuation v. maintenance of
antipsychotic medication on relapse rates
in patients with remitted/stable first-episode psychosis: a meta-analysis. Psychol Med. 2019;49(5):772–9. doi: 10.1017/S0033291718001393.
7. Guo
X, Zhang Z, Zhai J, Fang M,
Hu M, Wu R, et al. Effects of antipsychotic medications on quality of life and psychosocial functioning in patients with early-stage
schizophrenia: 1-year follow-up
naturalistic study. Compr Psychiatry. 2012;53(7):1006–12. Doi: 10.1016/j.comppsych.2012.03.003.
8. Hodgkin
D, Piazza M, Crisante M, Gallo C, Fiestas F. Availability of psychotropic medications in health care facilities of the Ministry of Health of Peru, 2011. Rev Peru Med
Exp Salud Publica. 2014;31(4):660–8.
9. Pennington
M, McCrone P. The Cost of Relapse in Schizophrenia. PharmacoEconomics.
2017;35(9):921–36. doi: 10.1007/s40273-017-0515-3.
10. Shukla
AK, Agnihotri A. Cost analysis of antipsychotic drugs available in India. Int J Basic Clin Pharmacol. 2017;6(3):669–74. doi: http://dx.doi.org/10.18203/2319-2003.ijbcp20170834.
11. Razzouk
D. Cost variation of antipsychotics in the public health system
in Brazil. J Bras Econ Saude. 2017;9((Suppl.1)):49–57. doi:
10.21115/JBES. v9.suppl1.49-57.
12. Defensoría del Pueblo.
Reporte Derecho a la salud [Internet]. Lima: Defensoría del Pueblo; 2018
[citado el 4 de julio de 2019]. Disponible en: https://www.defensoria.gob.pe/wp-content/uploads/2018/12/Reporte-Derecho-a-la-Salud.pdf.
13. Observatorio Peruano de
Productos Farmacéuticos [Internet]. Lima: Dirección General de Medicamentos,
Insumos y Drogas; 2019 [citado el 5 de julio de 2019]. Disponible en: http://observatorio.digemid.minsa.gob.pe/.
14. Ministerio de Salud.
Petitorio Nacional Único de Medicamentos esenciales para el sector salud
[Internet]. Lima: Dirección General de Medicamentos, Insumos y Drogas; 2015
[citado el 6 de julio de 2019]. Disponible en: http://www.digemid.minsa.gob.pe/UpLoad/UpLoaded/PDF/Normatividad/2018/RM_1361-2018.pdf.
15. Díez MV, Errecalde MF. Aclaraciones al concepto de genérico. Inf Ter Sist Nac
Salud. 1998;22(3):68–72.
16. Gardner DM, Murphy AL, O’Donnell H, Centorrino F, Baldessarini RJ. International consensus
study of antipsychotic dosing. Am J Psychiatry. 2010;167(6):686-93.
17. Ministerio de Salud.
Directiva Administrativa N°249- MINSA/2018/DIGEMID Gestión del sistema
integrado de suministro público de productos farmacéuticos, dispositivos
médicos y productos sanitarios-SISMED [Internet], 2018 [citado el 7 de julio de
2019]. Disponible en: http://www.digemid.minsa.gob.pe/UpLoad/UpLoaded/PDF/EAccMed/Normatividad/E03_RM_116-2018.pdf.
18. Huarag
E. ¿Un remedio peor que la enfermedad? sobre concentraciones, monopolios y
acceso a los medicamentos. Pluriversidad. 2018;1(1):111–26. doi:
10.31381/pluriversidad.v1i1.1674.
19. Kukreja
S, Kalra G, Shah N, Shrivastava A. Polypharmacy in psychiatry: a review. Mens Sana Monogr. 2013;11(1):82–99. doi:
10.4103/0973-1229.104497.
20. Stucchi-Portocarrero
S, Saavedra JE. Polifarmacia psiquiátrica en personas con esquizofrenia en un
establecimiento público de salud mental en Lima. Rev Neuro-Psiquiatr. 2018;81(3):145–53.
doi: 10.20453/rnp.v81i3.3382.
21. Bojórquez Giraldo E,
Arévalo Alván A, Castro Cisneros K, Ludowieg Casinelli L, Orihuela
Fernández S. Patrones de prescripción de psicofármacos en pacientes con
esquizofrenia y trastornos relacionados internados en el Hospital Víctor Larco
Herrera, 2015. An Fac Med. 2017;78(4):386–92. doi: 10.15381/anales.v78i4.14258.
22. Miranda J. El mercado de
medicamentos en el Perú ¿libre o regulado? Lima: Consorcio de Investigación
Económica y Social [Internet]. Lima: Ministerio de Economía y Finanzas; 2004
[citado el 10 de julio de 2019]. Disponible en: https://www.mef.gob.pe/contenidos/pol_econ/documentos/Medicamentos_competencia.pdf.
Funding
Sources:
Self-funded.
Citation:
Valle
R. Variabilidad de costos de antipsicóticos según establecimientos
farmacéuticos en Lima, Perú. 2020;37(1):67-73. Doi:
https://doi.org/10.17843/rpmesp.2020.371.4899.
Correspondence to:
Rubén Valle; Av. Alameda del
Corregidor 1531, La Molina, Lima 15024, Perú;
ruben_vr12@hotmail.com;
(511) 365-2300.
Authorship contributions:
VR conceived and designed the study, collected the data, analyzed
and interpreted the results, wrote the article and approved the final version.
Conflicts of Interest:
The author claims no conflict of interest.
20/10/2019
Approved:
12/02/2020
Online:
23/03/2020