Stefany Fiorella Infante Varillas
Heli Jaime Barrón Pastor
Yesica Llimpe Mitma
Doris Huerta Canales
Paolo Alberto Wong Chero
César Gutierrez
Silvia Suarez Cunza
10.17843/rpmesp.2020.373.4918
BRIEF REPORT
Immunological and biochemical response from older adults with urinary tract infection to uropathogenic Esherichia coli virulence factors
Arturo Octavio Gonzales-Rodriguez
![]() , Clinical Laboratory Technologist, Bachelor of Clinical Laboratory
Technology and Anatomical Pathology
, Clinical Laboratory Technologist, Bachelor of Clinical Laboratory
Technology and Anatomical Pathology
Stefany Fiorella Infante Varillas
![]() , Biologist-Microbiologist, Master in Biomedical Research
, Biologist-Microbiologist, Master in Biomedical Research
Heli Jaime Barrón Pastor
![]() , Medical Technologist in Clinical Laboratory, Doctor in Evolutionary
Ecology and Genetics
, Medical Technologist in Clinical Laboratory, Doctor in Evolutionary
Ecology and Genetics
Yesica Llimpe Mitma
![]() , biologist, Doctor of Biological Sciences
, biologist, Doctor of Biological Sciences
Doris Huerta Canales
![]() , biologist, Doctor of Biological Sciences
, biologist, Doctor of Biological Sciences
Paolo Alberto Wong Chero
![]() , Medical Doctor
, Medical Doctor
César Gutierrez
![]() , Medical Doctor, Master in Epidemiology
, Medical Doctor, Master in Epidemiology
Silvia Suarez Cunza
![]() , Pharmaceutical Chemist, Doctor in Pharmacy and Biochemistry
, Pharmaceutical Chemist, Doctor in Pharmacy and Biochemistry
ABSTRACT
Descriptive study in which 24 urine samples from older adults with urinary tract infection (UTI), from nursing homes, were evaluated; in order to identify differences in the immune and biochemical response from older adults with UTI by Escherichia coli (E. coli) to major virulence factors in the pathogenesis of UTI. Iron concentration, TNF-α, IL-1β and antioxidant capacity in urine were determined. A relation was found between, an increase in iron and red blood cell concentration in urine, and the presence of the pap GII gene found in E. coli. It is concluded that older adults, with UTIs by E. coli with the gene pap GII, have increased tissue damage.
Keywords: Nursing Homes; Elderly; Uropathogenic Escherichia coli; Biomarkers; Virulence Factors, Urinary Tract Infections, Immunology, Urine, Antioxidants, Cytokines (Source: MeSH NLM).
INTRODUCTION
Escherichia coli (E. coli) is the most frequent
cause of bacteremia in men and women (1), and the urinary tract
is the main way of infection in geriatric patients (2). This is
partially due to the fact that the older adult population (OAP) presents
particular immunological characteristics, and a subclinical state of chronic
inflammation, known as immunosenescence, where the polymorphonuclear lineage
(main line of defense in urinary tract infections [UTIs]) (3) has
limited function (4). Several E. coli virulence factors have
been described, mainly associated with bacteremia and sepsis, which include
cell adhesion molecules, iron uptake systems and exotoxins that form a protein
system that allows the bacteria to elude or injure the patient’s immune system (5,6).
The interaction between the immune system of patients with UTIs and the
genetic ability of the bacteria to form virulence factors determines the
bacterial clearance in the urinary tract (6), so it is necessary to
explore the difference in the immune and biochemical response of older adults
with UTIs to the various virulence factors associated with sepsis in
uropathogenic E. coli (UPEC).
|
KEY MESSAGES |
|
Motivation for the study: Older adults have an immunosenescent immune
system, so it is convenient to identify virulence factors in the bacteria
that can alter immune response. Main findings: The Escherichia coli carrier of the pap
GII gene induce greater tissue damage, which increases the
concentration of iron and red blood cells. Besides, there is a generalized
presence of nanA gene, which is important
for older adults during sepsis stages. Implications: The findings contribute to the study of the immunological response in
older adults with UTI, and it is the first report in Peru about the frequency
of virulence factors in uropathogenic Escherichia
coli in gerontological nursing homes. |
THE STUDY
Between April and July 2018, the urine of 24 older adults with UTIs, of
both sexes, residing in private gerontological nursing homes in Lima, was
evaluated. The diagnostic criteria for UTIs were defined as: a microscopic
count of >5 leukocytes per field of 400x magnification, the conversion of
nitrites by the Griess method and a count of more than 100,000 colony-forming
units in the blood agar culture medium. Urine sediment analysis was
standardized according to the recommendations of the Chilean Health Institute (7).
The etiological agent was identified by using traditional biochemical
methods and the bacteria identified as E. coli were preserved in tryptic
soy broth and 20% glycerol. Polymicrobial cultures were excluded from the
study. Subsequently, the bacterial DNA was extracted using the GeneJet Genomic kit (Thermo
Scientific®, Massachusetts, USA) and the presence of 11 virulence genes was
evaluated: aer, α-hly,
cnf-1, sfa, chuA, TcpC, nanA, pap GI, GII,
GIII and iucC by end-point polymerase
chain reaction.
The urine samples were centrifuged at 3,000 g (Sigma, 3-30KS) for
10 minutes, preserving the supernatant. Concentrations of TNF-α, IL-1β and iron
were determined; besides, the total antioxidant capacity in urine was evaluated
by ABTS•+ and FRAP methods, which acted as immune response markers
through the increase of reactive oxygen substances (ROS). All analytes were
measured using the Multiskan Go spectrophotometer (Thermo Scientific®, Massachusetts, USA).
The statistical analysis was carried out with the Epidat
version 4.1 program. The description of the qualitative variables was made
through frequency tables. Shapiro Wilk’s normality test was applied to
determine the distribution of quantitative variables and Levene’s
test was used to evaluate the variance homogeneity of the variables. The
quantitative variables with normal distribution were analyzed by means of the
Student’s T test. p values <0.05 were considered
significant.
This study was approved by the Ethics Committee of the Faculty of
Medicine of the Universidad Nacional Mayor de San Marcos, act 1812 with project
code 0013.
FINDINGS
Twenty-four urine samples from older adults with UTIs by E. coli,
from gerontological nursing homes, were analyzed. The most frequent virulence
genes were nanA, pap GII, aer, chuA and iucC. Genes α-hly and cnf-1 were found in low proportion
and the following genes were not found: TcpC,
pap GI, pap GIII and sfa (Figure 1).
Met: Metabolism
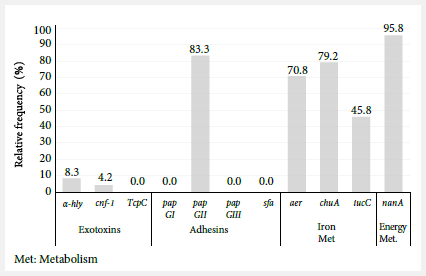
Figure 1. Relative
frequency of virulence genes in uropathogenic Escherichia
coli in older adults from nursing homes.
Regarding the immune and biochemical response of older adults to the
various virulence genes evaluated, a concentration of
37.6 red blood cells/μL and 193.4 μg/L
of iron was observed in patients carrying the pap GII gene, values
were significantly higher in patients infected with E. coli, but without
this gene. In addition, patients with strains carrying the pap GII gene
showed a positive tendency towards having a higher urine antioxidant capacity regarding
the ABTS•+ test (1348.7 vs. 634.8 Eq-real Vit C μg/mL) (Table 1). On the
other hand, a higher concentration of leukocytes (p = 0.070) was observed in
patients infected with E. coli carriers of the three genes related to
iron metabolism evaluated (iucC, aer and chuA) (Table 2).
Table 1. Immunological and biochemical markers compared to the presence of the pap GII gene.
|
Immunological and biochemical markers |
Presence of pap GII a |
Absence of pap
GII a |
p value b |
|
Leucocytes/μL |
270.1 ± 240.7 |
225.8 ± 126.0 |
0.729 |
|
Red blood cells/μL |
37.6 ± 37.4 |
12 ± 8.2 |
0.010 |
|
Iron (μg/L) |
193.4 ± 139.6 |
85.3 ± 26.2 |
0.004 |
|
IL-1β (pg/mL) |
375 ± 293.2 |
147 ± 98.8 |
0.144 |
|
TNF- α (pg/mL) |
65.2 ± 35.0 |
94.5 ± 61.5 |
0.195 |
|
ABTS Eq- real Vit C (μg/mL) |
1348.7 ± 1455.7 |
634.8 ± 299.0 |
0.059 |
|
FRAP (mM) |
1.006 ± 0.416 |
0.801 ± 0.332 |
0.366 |
a media ± desviación estándar;
b prueba T de Student
FRAP: Recuperación
de fluorescencia después de
photobleaching, ABTS: Ácido
2,2’-azino-di-(3-etilbenzotiazolina)-6-sulfónico
Table 2. Immunological and biochemical markers compared
with the presence of iucC+aer+chuA
genes.
|
Immunological and biochemical markers |
Presence of iucC+aer+chuA a |
Absence of iucC+aer+chuA a |
p value b |
|
Leucocytes/μL |
391.7 ± 226.6 |
209.6 ± 206.5 |
0.070 |
|
Red blood cells/μL |
35.3 ± 36 |
32.6 ± 36.4 |
0.903 |
|
Iron (μg/L) |
210.6 ± 140.2 |
160.9 ± 132.6 |
0.418 |
|
IL-1β (pg/mL) |
421.1 ± 280.5 |
302.4 ± 284.4 |
0.359 |
|
TNF - α (pg/mL) |
82.8 ± 24.2 |
64.9 ± 45 |
0.332 |
|
ABTS Eq- real Vit C (μg/mL) |
1763.7 ± 2349.6 |
1009.9 ± 626.8 |
0.435 |
|
FRAP (mM) |
0.957 ± 0.307 |
0.978 ± 0.447 |
0.911 |
a Mean ±
standard deviation; b Student’s T-test.
FRAP: Fluorescence recovery after photobleaching, ABTS: 2,2'-Azino-di-(3-ethylbenzothiazoline)-6-sulfonic
acid.
DISCUSSION
This study evaluated the immune and biochemical response in the urine of
hospitalized older patients infected by UPEC (the main etiological agent of
UTIs). One of the main findings was that the presence of the pap GII
gene induced hematuria and a higher iron concentration in the urine. The
frequency of virulence genes important in the pathogenicity process of UTIs was
also evaluated. Another important finding was that 95.8% of UPEC presented the nanA gene.
N-acetylneuraminic acid, an important substrate in the energetic
production of E. coli, is split by the N-acetylneuraminic
lyase (nanA) enzyme into
pyruvate and N-acetyl-D-manosamine (8).
The presence of nanA enzyme generates high
competitiveness in the bacteremia-producing UPEC; and although its function in
UTI pathogenesis in murine models is less relevant (8), results
indicate the existence of a high risk of developing sepsis in older adults with
bacteremia.
On the other hand, exotoxins have a role in the pathogenesis of UTIs.
Neutrophils, the main line of defense in UTIs, are lysed by high doses of α-hemolysin (HlyA) and, in
addition, bladder cells in low doses are exfoliated (9), which
deteriorates the body’s two main lines of defense (3). Nevertheless,
we obtained a frequency of 8.3% in the studied UPEC, which is lower than what
was found in other studies carried out in geriatric population (10,11). Likewise, the exotoxins, such as the necrotizing
cytotoxic factor type 1 (CNF1) genetically related to HlyA,
induce a rearrangement of the neutrophilic cytoskeleton through the activation
of the Rho GTPase type enzymes (9). In accordance with what was
reported by α-hly, we found a UPEC carrier of
the cnf-1 gene.
The TcpC protein recently described as
interfering in the production of proinflammatory cytokines in the UTI (12)
was not found in any of the evaluated UPEC, which may reflect the absence of
the type IV pathogenicity island, dependent on its horizontal transfer, or the
recent evolutionary acquisition of the gene in extra-intestinal E. coli (12).
Regarding the immunological and biochemical response observed in the older
adults, iron is scarce in the urinary fluid and is indispensable for bacterial
metabolism (13,14), the microorganisms that
infect the urinary tract must have the capacity to capture and compete for iron
assimilation (14). UPECs have three systems of iron uptake (siderophores, hemophores and
direct iron uptake in its ferrous state), which are reported to have increased
expression in vivo (15). On the other hand, iron restriction
is an immune defense mechanism used by the host to limit bacterial
proliferation (16). Although we could not find significant
differences between immunological and biochemical markers and genes associated
with iron metabolism, it can be observed that patients with UPEC, carriers of
the iucC, aer
and chuA genes, tend to have higher leukocyte concentrations,
which may indicate a greater immune stress. Besides, the presence of chuA gene and other siderophore systems are highly
concentrated in strains that cause recurrent UTI (17), a common
situation in gerontological resting centers.
Finally, the pap GII gene is a virulence factor whose
function is to ensure the adhesion of UPEC to renal tissue. The association of pap
GII gene with pyelonephritis stages has been documented (6), besides, it has been proposed that it confers competitive
advantage during bacteremia stages by UTI (8). Some evidence
indicates that its presence is not determinant in stages of pyelonephritis,
therefore, its function is not yet conclusive in the process of infection in
the urinary tract (18).
Results obtained show that patients with UPEC positive for the pap
GII gene had higher iron concentration compared to patients with UPEC
negative for the pap GII gene. It has been found that the
interaction of pap GII with its receptor induces rapid transcription of
the airS gene in UPEC in urine, which has a
fundamental role in the activation of the siderophore
systems (aerobactin/enterobactin)
(19) by decreasing the concentration of iron in urine. In the
results obtained we did not find this association. However, this could be
explained by the higher concentration of red blood cells and hemolysis in this
group of patients. The adhesion of the pap GII protein activates the
synthesis of cytokines (20), causing the rupture of blood vessels
located in the lamina itself. On the other hand, the ABTS•+ test
describes that in patients with positive pap GII UPEC there is a
tendency to have greater antioxidant capacity, which could be due to higher iron
concentration, which interferes with the assay, although, this tendency could
also be explained by the deficiency of neutrophils to produce reactive oxygen
substances. Recent studies have described an increase in the neutrophil
subpopulation CD16/CD62L in the OAP, which presents a lower level of response
to cytokine stimuli (4).
This study has several limitations. First, it was not possible to record
information from the patients regarding their clinical condition, infection
stage, use of antibiotics, infection recurrence. Second, the low number of
urine samples analyzed, which increases the probability of obtaining a type II
error. Third, we do not complement our studies with gene expression analysis,
so we do not know if the genes evaluated are indeed expressed by the bacteria.
In conclusion, E. coli carrying the pap GII gene can
induce greater tissue damage that possibly favors a higher iron concentration
in the urine, which stimulates its increase. In addition, patients infected
with E. coli with pap GII show a positive tendency to have
greater antioxidant capacity, which may be due to the deficiency of neutrophils
recruited in the OAP during the production of ROS. Finally, the generalized
presence of nanA gene is important due to its
high relevance in sepsis stages.
REFERENCES
1. Nicolle LE. Urinary Tract Infections in the Older Adult. Clin Geriatr Med. 2016;32(3):523-38. doi: 10.1016/j.cger.2016.03.002.
2. Mylotte JM, Tayara A, Goodnough S. Epidemiology of Bloodstream Infection in Nursing Home Residents: Evaluation in a Large Cohort from Multiple Homes. Clin Infect Dis. 2002;35(12):1484-90. doi: 10.1086/344649.
3. Luna-Pineda VM, Ochoa S, Cruz-Córdova A, Cázares-Domínguez V, Vélez-González F, Hernández-Castro, R, et al. Infecciones del tracto urinario, inmunidad y vacunación. Bol Med Hosp Infant Mex. 2018; 75(2): 67-78. doi: 10.24875/BMHIM.M18000011.
4. Sauce D, Dong Y, Campillo-Gimenez L, Casulli S, Bayard C, Autran B, et al. Reduced oxidative burst by primed neutrophils in the elderly individuals is associated with increased levels of the CD16bright/CD62Ldim immunosuppressive subset. J Gerontol A Biol Sci Med Sci. 2017;72(2):163-72. doi: 10.1093/gerona/glw062.
5. Daga AP, Koga VL, Gabriel J, Soncini M, Matos CM De, Regina M, et al. Escherichia coli Bloodstream Infections in Patients at a University Hospital : Virulence Factors and Clinical Characteristics. Front Cell Infect Microbiol. 2019;9:191. doi: 10.3389/fcimb.2019.00191.
6. Johnson JR. Virulence factors in Escherichia coli urinary tract infection. Clin Microbiol Rev. 1991; 4(1):80-128. doi: 10.1128/cmr.4.1.80.
7. Gómez R, Pellegrini P. Recomendaciones para el Ánalisis del Sedimento urinario. Departamento Laboratorio Biomédico Nacional y de Referencia. Instituto Nacional de Salud Pública de Chile. 2013 [citado el 03 de mayo de 2020]. Disponible en: https://www.araucaniasur.cl/wp-content/uploads/2019/11/sedimento-urinario 10052013A.pdf.
8. Smith SN, Hagan EC, Lane MC, Mobley HLT. Dissemination and Systemic Colonization of Uropathogenic Escherichia coli in a Murine Model of Bacteremia. MBio. 2010;1(5):1–9. doi: 10.1128/mBio.00262-10.
9. Lüthje P, Brauner A. Virulence Factors of Uropathogenic E. coli and Their Interaction with the Host. Adv Microb Physiol. 2014;65:337-72. doi: 10.1016/bs.ampbs.2014.08.006.
10. Santo, E, Macedo C, Marin JM. Virulence factors of uropathogenic Escherichia coli from a University Hospital in Ribeirão Preto, São Paulo, Brazil. Rev Inst Med Trop Sao Paulo. 2006;48(4):185-88. doi: 10.1590/s0036-46652006000400002.
11. Croxall G, Hale J, Weston V, Manning G, Cheetham P, Achtman M, et al. Molecular epidemiology of extraintestinal pathogenic Escherichia coli isolates from a regional cohort of elderly patients highlights the prevalence of ST131 strains with increased antimicrobial resistance in both community and hospital care settings. J Antimicrob Chemother. 2011;66(11):2501-8. doi: 10.1093/jac/dkr349.
12. Xiao T, Waldhuber A, Svanborg C, Snyder G, Römmler F, Miethke T, et al. A Comparative Analysis of the Mechanism of Toll-Like Receptor-Dis-ruption by TIR-Containing Protein C from Uropathogenic Escherichia coli. Pathogens. 2016;5(1):25. doi: 10.3390/pathogens5010025.
13. Pfrimer K, Micheletto RF, Marchini JS, Padovan GJ, Moriguti J, Ferriolli E. Impact of Aging on Urinary Excretion of Iron and Zinc. Nutr Metab Insights. 2014;7:47-50 doi: 10.4137/NMI.S12977.
14. Alteri CJ, Smith SN, Mobley HLT. Fitness of Escherichia coliduring urinary tract infection requires gluconeogenesis and the TCA cycle. PLoS Pathog. 2009;5(5):e1000448. doi: 10.1371/journal.ppat.1000448.
15. Hagan EC, Lloyd AL, Rasko DA, Faerber GJ, Mobley HLT. Escherichia coli global gene expression in urine from women with urinary tract infection. PLoS Pathog. 2010; 11;6(11): e1001187. doi: 10.1371/journal.ppat.1001187.
16. Bullen JJ. The Significance of Iron in Infection. Clin Infect Dis. 1981;3(6):1127-38. doi: 10.1093/clinids/3.6.1127.
17. Ejrnæs K, Stegger M, Reisner A, Ferry S, Monsen T, Holm SE, et al. Characteristics of Escherichia coli causing persistence or relapse of urinary tract infections: Phylogenetic groups, virulence factors and biofilm formation. Virulence. 2011;2(6):528-37. doi: 10.4161/viru.2.6.18189.
18. Mobley HLT, Jarvis KG, Elwood JP, Whittle DI, Lockatell CV, Russell RG, et al. Isogenic P-fimbrial deletion mutants of pyelonephritogenic Escherichia coli: the role of alpha Gal(1-4) beta Gal binding in virulence of a wild-type strain. Mol Microbiol. 1993;10(1):143–55. doi: 10.1111/j.1365-2958.1993.tb00911.x.
19. Zhao R, Shi J, Shen Y, Li Y, Han Q, Zhang X, et al. Phylogenetic distribution of virulence genes among ESBL-producing uropathogenic escherichia coli isolated from long-term hospitalized patients. J Clin Diagnostic Res. 2015;9(7):1-4. doi: 10.7860/JCDR/2015/13234.6157.
20. Svensson M, Duan R, Svanborg C. Role of the Ceramide-sig-naling Pathway in Cytokinr Responses to P-fimbriated. J Exp Med. 1996;183(3):1037-44. doi: 10.1084/jem.183.3.1037.
Correspondence to: Arturo Gonzales Rodriguez; calle Mártir José Olaya 162, Miraflores, Lima, Perú; arturo. gonzales@udep.edu.pe.
Authors’ contributions: AGR, HJBP, YLLM and DVRC conceived of the article. AGR, CG, SFIV, PW,
HJBP and YLLM collected the data and did the statistical analysis. AGR, PW,
HJBP and SSC wrote and approved the final version.
Conflicts of interest: The authors declare no conflict of interest.
Funding sources: Funding for research groups from the
Universidad Nacional Mayor de San Marcos (project code A17011681) and internal
funding from the Universidad de Piura.
Cite as:
Gonzales-Rodriguez AO, Infantes Varillas
SF, Barrón Pastor HJ, Llimpe
Mitma Y, Huerta Canales D, Wong Chero
PA, et al. Immunological and biochemical response of older adults with
urinary tract infection to uropathogenic Escherichia
coli virulence factors. Rev Peru Med Exp Salud Publica. 2020;37(3):527-31. doi:
https://doi.org/10.17843/rpmesp.2020.373.4918.