Dedsy Yajaira Berbesí-Fernández
Sebastián Bedoya-Mejía
Amanda Patricia Molina-Estrada
Alejandra Martínez-Rocha
Ángela M Segura-Cardona
Original article
Factors associated with the perception of HIV vulnerability among transgender women in three Colombian cities
Sara Milena Ramos-Jaraba ![]() 1, Health Administrator; Master in Collective Health
1, Health Administrator; Master in Collective Health
Dedsy Yajaira Berbesí-Fernández ![]() 1, Nurse; Doctor in Epidemiology and Biostatistics
1, Nurse; Doctor in Epidemiology and Biostatistics
Sebastián Bedoya-Mejía ![]() 2, Manager of Health Information Systems; Database and Information Security Specialist
2, Manager of Health Information Systems; Database and Information Security Specialist
Amanda Patricia Molina-Estrada ![]() 1, Nurse; Master in Epidemiology
1, Nurse; Master in Epidemiology
Alejandra Martínez-Rocha ![]() 1, Veterinarian; Master in
Public Health
1, Veterinarian; Master in
Public Health
Ángela M Segura-Cardona ![]() 2, Statistician; Doctor in Epidemiology
2, Statistician; Doctor in Epidemiology
1 Facultad de Enfermería, Universidad CES, Medellín, Colombia.
2 Escuela de Graduados, Universidad CES, Medellín, Colombia.
ABSTRACT
Objective: To describe the perception of vulnerability to HIV and its associated factors among transgender women (TW) in Bogotá, Medellín and Santiago de Cali, Colombia.
Materials and methods: We conducted a cross-sectional study, using respondent-driven sampling (RDS) in which 620 TW participated. Sociodemographic aspects, sexual behavior, consumption of psychoactive substances and the perception of vulnerability to HIV were studied. We carried out a descriptive analysis, in which bivariate associations were evaluated using chi-square. We also conducted a multivariate analysis and built a model using Poisson regression.
Results: Of the participants, 63% were 35 years old or younger, had low income, started sexual relations at an early age and worked mainly as sex workers, webcam models and hairdressers; 84.7% of the participants had received money in exchange for sex at some point. The perception of vulnerability to HIV increased among those who were single, worked in prostitution, had sexually transmitted infections in the last year, avoided preventive health services and consumed cocaine during the six months before this survey.
Conclusion: The perception of vulnerability to HIV among the TW participants in this study is high; therefore, effective interventions are required to improve the living conditions and sexual behavior of this population.
Keywords: HIV; Vulnerable Populations; Transgender Persons; Colombia (source: MeSH NLM).
INTRODUCTION
Human immunodeficiency virus (HIV) infection is a public health problem worldwide, which has caused 39 million deaths; currently about 36 million people live with HIV. It is estimated that about 35,000 deaths and 100,000 new infections occurred in Latin America in 2017 (1). In Colombia, the age-adjusted HIV prevalence for 2019 was 0.19 per 100,000 inhabitants, while in other groups, such as men who have sex with men (MSM), transgender women (TW), people who inject drugs and street dwellers, it is over 5% (2).
These differences in the distribution of the HIV epidemic according to population groups and the increase in the number of new cases in the world led to the epidemic being explained in terms of vulnerability in the early 1980s (3). This concept allows for a better understanding of the individual and collective determinants immersed in the health-disease process (4-5).
In this sense, the term vulnerability is understood as the susceptibility of the subject to becoming ill, resulting from a set of sociocultural, epidemiological, psychobiological factors, relocating the subject in his/her relationship with the collective (6). Under this perspective, several studies have explained the incidence and prevalence of HIV in TW through some complex individual factors: biological (use of hormonal therapy that could interact with antiretroviral treatment or with drugs used for HIV pre-exposure prophylaxis) and behavioral (sexual intercourse without condom use and the use of psychoactive substances). In addition, structural and social factors can influence behaviors, practices and attitudes that increase vulnerability to HIV, limiting aspects such as access to socioeconomic resources, especially education, work and prevention services (7).
Similarly, the experience of TW has been affected by violence and exclusion in several regions of the world. Various studies have reported that factors that increase the vulnerability of TW to HIV infection are related to violence, including hate crimes, physical and sexual abuse, gender discrimination associated with sexual risk behaviors, alcohol consumption and use of other psychoactive substances, mental health problems such as depression with suicidal ideation and attempts, as well as high rates of sexually transmitted infections (STIs) such as syphilis, hepatitis B, human papillomavirus (HPV), and herpes simplex virus (HSV) (7-9).
Some studies have estimated that 19% of TW have HIV and that they are up to 49 times more likely to acquire it than all adults of reproductive age, and a much higher prevalence has been reported compared to self-identified MSM (10). In high-income countries, a prevalence of 22% has been reported, with TW of African descent being the most affected (7). Some studies indicate that prevalence in Asia-Pacific regions is as high as 49% (11), in Peru it has been reported to be 30% (12), and in Argentina 34% (13). In Colombia, studies on seroprevalence, sexual behavior, and vulnerability of TW carried out in several cities in 2012 and 2016 reported an overall prevalence of HIV infection of 15% and 21.3%, respectively (14). Thus, TW are disproportionately affected and constitute the population with the highest vulnerability to HIV strongly related to stigma and prejudice.
Although some authors have raised the discussion of vulnerability to HIV as a crucial issue for the analysis of the phenomenon in TW, in Colombia there are few quantitative studies on the subject, so questions remain about how to focus prevention actions that include the needs and perceptions of the women themselves. The aim of this study was to describe the perception of vulnerability to HIV and its associated factors in the TW that participated in the sampling conducted in Bogotá, Medellín and Cali.
|
KEY MESSAGES |
|
Motivation for the study: In Colombia and Latin America, there is high prevalence of HIV among transgender women (TW), which is considered a priority group for public health intervention. However, there are few quantitative studies that address social, individual and political factors, which may be related to vulnerability to HIV/AIDS. Main findings: TW have a high perception of vulnerability to HIV, and factors associated with this vulnerability involve engaging in multiple sexual risk behaviors, consuming psychoactive substances, and working in prostitution. Implications: Contextualized interventions are required, with intersectional and participatory approaches, within the framework of human rights guarantees, which can contribute to the transformation of individual, social and programmatic vulnerability to HIV infection. |
MATERIALS AND METHODS
Type of study and population
A cross-sectional study was carried out in the cities of Bogota, Medellin and Cali, between May and September 2019; 620 TW participated. Due to the characteristics of the study population, it was not possible to have a sampling frame that would allow the design of a conventional probability sample, so we opted for respondent-driven sampling (RDS), a method that has proven useful in hard-to-reach populations. This sampling uses social network theory, utilizing a reference chain as a method for controlled data collection (15).
Recruitment
Recruitment began with 20 initial participants or seeds, who were identified by formal and informal interviews with key members of the population, and by the experience of the research team. We selected those who expressed the ability to convene a large group of TW, who had leadership, visibility, recognition, credibility and met the minimum eligibility criteria. The seeds received three coupons to invite other TW in their network to participate in the study; each new participant who entered the study referred by one of the seeds was again given three coupons; this chain recruitment system was continued until the total number of participants was reached. Following the RDS theory, each person was given an incentive for their participation in the study (change from Colombian pesos to dollars in 2019), which was a supermarket voucher (40,000 COP, approximately 12 USD) and a secondary cash voucher linked to the successful recruitment of three new participants (30,000 COP, approximately 9 USD).
The sample size was reached within eighteen weeks. The inclusion criteria for all participants were the assignment of male sex at birth, identification with the female gender, being older than 18 years, residing in the cities of Bogotá, Medellín (metropolitan area) and Cali (metropolitan area) and presenting an invitation coupon given to them by a person who had participated.
Procedure
We applied a survey, adapted to the guidelines for repeated behavioral surveys in populations at risk of acquiring HIV, which was adjusted in Colombia by a group of experts from the funding entity (16). This survey was applied digitally, the data were controlled by validators, all fields were mandatory and no missing data were reported. The survey was divided into 12 sections: social and demographic characteristics, health and access to services, body transformations, sexual history, sexually transmitted infections, sex work, condoms and lubricant, knowledge about HIV/AIDS, HIV exposure, intervention and testing, psychoactive substance use, social networks and stigma/discrimination. The outcome variable was the perception of vulnerability to HIV, measured with the question "How would you assess the degree of vulnerability or risk that you have of becoming infected with HIV?", the reference category was low vulnerability versus medium-high vulnerability. Initially, we considered three categories regarding the analysis of vulnerability to HIV (low, medium and high) according to the question asked to the TW, but because of having such a low proportion in one category (high) we proceeded to join the category of medium-high vulnerability (58.3%) and compare it with low vulnerability (39.9%). The control variables of the study were age, educational level, occupation, marital status, socioeconomic stratum, health insurance, income, knowledge of HIV, age at first sexual intercourse, sexually transmitted infections in the last year, having an HIV test in the last year, HIV diagnosis, discrimination in the last year, avoidance of seeking prevention services, money in exchange for sex, cocaine and marijuana use in the last 6 months.
Statistical analysis
We described the characteristics of TW and carried out Chi-square analyses. In order to explore the factors associated with the perception of vulnerability to HIV, the association of such vulnerability with the independent variables was assessed by using the prevalence ratio (PR), with a 95% confidence interval. We constructed a Poisson regression model, a log link and a robust estimator for the multivariate analysis; in the model we included the variables that were considered significant (p < 0.05) during the bivariate analysis and those that had no collinearity between them after a literature review on the subject. The SPSS 24.0 statistical package was used for the statistical analysis of the data.
Ethical Aspects
This article is derived from a national study entitled: "Vulnerability to HIV and HIV prevalence in transgender women in three cities of Colombia: Bogota, Medellin and Santiago de Cali, 2019". It was approved by the ethics committee of Universidad CES, in session of February 19, 2019, and was approved as minimal risk (Acta N.o 130 de 2019).
RESULTS
Out of the 620 TW, 36.5% lived in Bogotá, 32.8% in Medellín and 30.7% in Cali. The average age of the participants was 31 years in Medellín, 38 in Bogotá, 41 in Cali. The predominant marital status was single (79.8%), and the remaining 20.2% were married or in a common-law relationship. Out of the total, 68.5% had secondary education, followed by 15.5% with none or only primary education; 10.8% were technicians or technologists and a smaller percentage had a university or postgraduate degree (5.2%). Regarding the employment of TW, about half (50.2%) were engaged in sex work or offered web cam services, followed by 21%, who were stylists or dressmakers, 17.7% were employed or self-employed and 11.1% did not work or study (Table 1). Regarding their economic situation, 50.3% had low income, i.e., received minimum wage or less (minimum wage in 2019 is approximately 258 USD), and 11.5% received nothing.
Table 1. Sociodemographic, behavioral, and clinical characteristics according to HIV vulnerability (n = 620).
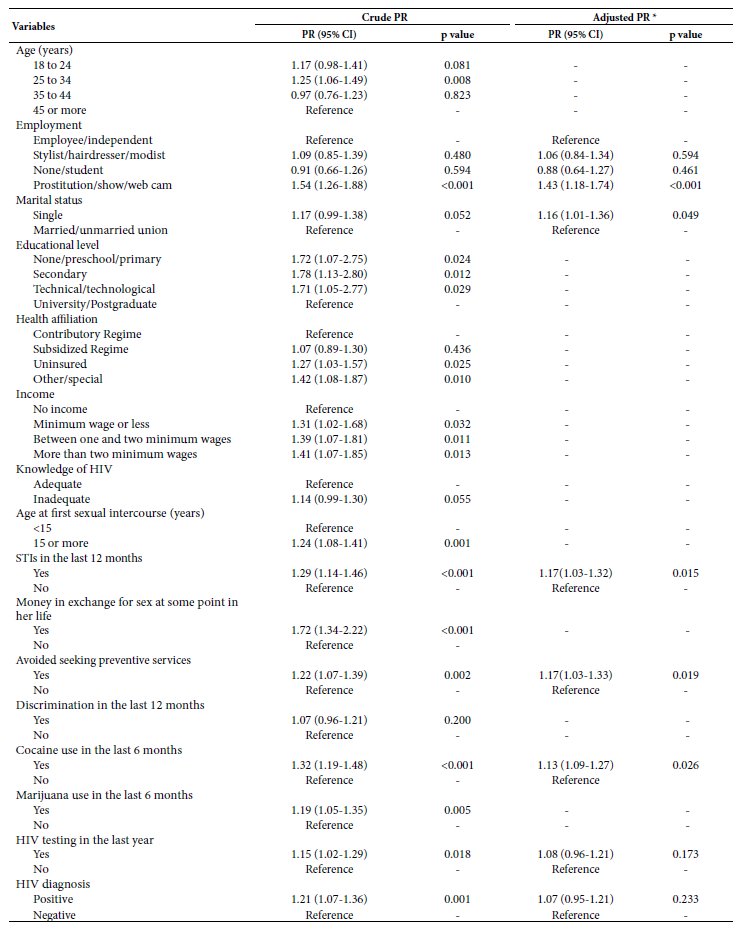
* Chi-square test.
STI: sexually transmitted infections.
Inadequate knowledge about HIV was found in 68.5% of the TW, only 13.4% reported having had an STI in the last year, and a considerable percentage (84.7%) had received money in exchange for sex at some point in their lives. Seeking HIV prevention, testing or treatment services was avoided in 15.8% of TW, and 45% felt discriminated against in the past year. When asked about the use of psychoactive substances in the last 6 months, more than half reported having smoked marijuana (58.1%), and 35.2% reported having used cocaine. A total of 50.6% had not been tested for HIV in the last year, and 22.6% were positive in the confirmatory test for HIV (Table 1).
Women who are perceived to be more vulnerable to HIV infection are younger, those who engage in prostitution or offer web cam services, are unmarried, have lower level of education, higher income, have inadequate knowledge of HIV, began sexual relations before age 15, avoid seeking prevention services, have received money in exchange for sex, use cocaine or marijuana, and those who have had an HIV test in the past year and tested positive for HIV infection.
In the adjusted model (Table 2), we found that the TW who perceive themselves more vulnerable to HIV are those who practice prostitution or offer web cam services, compared to those who are employed or independent (PR 1.43; 95% CI: 1.18-1.74); likewise, those who reported having had an STI in the last year had a 15% greater probability of feeling vulnerable to HIV in relation to those who have had an STI (PR 1.15; 95% CI: 1.02-1.31). Similarly, this probability increases among single women by 16% compared to married and cohabiting women (PR 1.16; 95% CI: 1.01-1.36), those who avoid seeking HIV prevention services (PR 1.17; 95% CI: 1.03-1.33) and cocaine users (PR 1.13; 95% CI: 1.09-1.27).
Table 2. Factors associated with perceived vulnerability to HIV in transgender women.
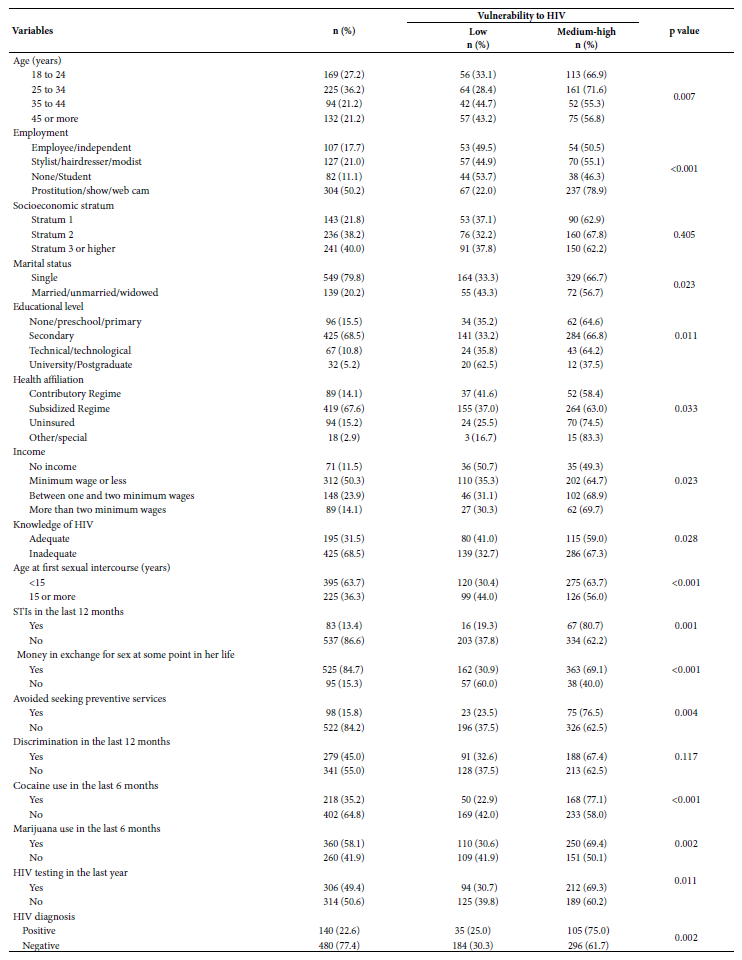
* Variables that presented collinearity with other variables, measured by Pearson’s correlation coefficient, were excluded: HIV test in the last year with age (0.664), knowledge of HIV (0.829) and money in exchange for sex once in life (0.421); STI in the last 12 months correlated with educational level (0.820), discrimination in the last 12 months (0.619), marijuana use in the last 6 months (0.724) and health affiliation (0.591); income correlated with avoidance of seeking prevention services (0.571) and HIV diagnosis (0.774); age at first intercourse correlated with HIV testing (0.954) and HIV knowledge (0.805).
STIs: sexually transmitted infections; PR: prevalence ratio.
DISCUSSION
This study found that more than half of TW perceive themselves as vulnerable to HIV, share precarious socioeconomic characteristics, and engage in risky sexual practices, as described in international literature, which reveals once again that TW live marginalized and vulnerable from a social point of view (10,16,17). It is important to understand HIV in the context of vulnerability because there are political, social and cultural aspects that negatively influence the decisions and lifestyles of TW, thus restricting their rights and decision-making guarantees.
Under the model proposed by Ayres (18), the individual dimension includes the lifestyles of the individuals, which may contribute to their exposure to the virus or, on the contrary, to their protection. In the case of the TW in our study, this dimension is reflected in their limited knowledge regarding HIV, early initiation of sexual relations, marijuana and cocaine use, and STIs acquired in the last year. In the collective dimension, the health-disease-care process is understood as a social process, whose content and quality of information are configured within a life in society and is expressed in the individual. We found that most of the participants worked as prostitutes or offered webcam services, had received money in exchange for sex at some time in their lives, had a low level of education, had low income, and belonged to the subsidized health regime (public health insurance), which corroborates that few TW have managed to break the barriers imposed by society and leave these schemes. The programmatic dimension, defined as national and local actions to combat HIV, are complex to address in this study; however, a significant percentage of TW avoid seeking HIV prevention activities or participating in them, which is a worrisome situation (18-19).
In a society in which differences are not accepted and with a predominant heteronormative discourse, i.e., male and female roles are clearly differentiated, being a TW is a cause of stigma and discrimination at all social levels. For this study, about 45% of discrimination cases were reported in the last year. This in turn reduces the possibilities of reaching high levels of education or having a stable or dignified job, and drives the population to engage in sex work as one of the few sources of income available, as reflected in this study (20,21).
These social, cultural, and gender conditions have a particular connotation in their lifestyles, as TW tend to consume high amounts of psychoactive substances, which is probably associated with prostitution or marginalization, which becomes a factor that increases the probability of contracting HIV (22). This is relevant because in this study cocaine and marijuana use was found to be associated with a high perception of vulnerability to HIV; similar results have been reported by other researchers, who found high prevalence of drug use in TW and generally higher in comparison with other populations, especially for these types of drugs (23). For example, in TW from San Francisco the prevalence of drug use was 43.3% (24); in New York, 76.2% (25); and in Brazil about 60% of transgender youth reported using cannabis, tranquilizers, and cocaine (26).
Furthermore, TW perceived greater vulnerability to HIV when they were diagnosed with an STI in the last year, which may be related to low or inconsistent condom use and drug use. It is known that TW have few opportunities to make decisions about their own bodies and to demand condom use with clients or steady partners. A study conducted in Colombia concluded that there is greater sexual vulnerability among TW who engage in prostitution, related to the fact that some associate the female role with a lack of autonomy and decision-making, a product of the structure of social and gender inequity (27). Similarly, several studies show high rates of STIs in TW, especially syphilis and gonorrhea (28).
Regarding health services, it is noteworthy that about 15% of TW avoid seeking prevention services, HIV testing and treatment, which makes them more vulnerable. Some studies conclude that in most Latin American countries there are insufficient and inadequate social and health services for TW; in addition, negative attitudes, stigma and discrimination from health service providers toward transgender persons limit acceptance, quality and access to promotion and prevention services (28-29). This situation also contributes to inadequate knowledge of HIV, as reported in this study (68.5%), because although prevention transcends institutional health spaces, these are an important reference to provide accurate information, continuity of care in case of a positive diagnosis and seek comprehensive solutions to all the problems that are interrelated and create greater vulnerability (30).
As a limitation of this study, we can mention that respondent-based sampling is considered a type of non-random selection that must meet a series of assumptions to be considered a social network-dependent sample. In addition, these data were obtained from a survey on sexual practices and condom use; the accuracy of which depended on the sincerity of the participant. As this is a cross-sectional investigation, neither temporal sequence nor causality could be established.
According to the findings of this research, it is important to build guidelines and procedures to care for the health of transgender people with a differential approach throughout the country; health services should be sensitized and familiarized with the specific health needs of this group, in order to avoid stigmatization. At the same time, interventions focused on the reduction of risk behaviors provided by health providers should be improved, since the implementation of strategies in the community and creating protective environments can increase attendance to social, health, psychological and legal services, and thus encourage condom use and improve other sexual behaviors.
REFERENCES
1. UNAIDS. Global HIV and AIDS statistics [Internet]. Reino Unido [citado el 9 de noviembre de 2019]. Disponible en: https://www.avert.org/global-hiv-and-aids-statistics.
2. Cuenta de Alto Costo. Situación del VIH Sida en Colombia. Bogotá: Cuenta de Alto Costo; 2019 [Internet]. Colombia; 2019 [citado el 9 de noviembre de 2019]. Disponible en: https://cuentadealtocosto.org/site/vih/situacion-del-vih-sida-en-colombia-2018/.
3. Busso G. La vulnerabilidad social y las políticas sociales a início del siglo XXI: uma aproximación a sus potencialidades y limitaciones para los países latino americanos. Santiago: CEPAL/Celad [Internet]. 2001 [citado el 9 de noviembre de 2019]. Disponible en: http://www.derechoshumanos.unlp.edu.ar/assets/files/documentos/vulnerabilidad-social-nociones-e-implicancias-de-politicas-para-latinoamerica-a-inicios-del-siglo-xxi.pdf.
4. Icumi Nichiata L, Bertolozzi MR, Ferreira Takahashi R, Aparecida Fracolli L. La utilización del concepto "vulnerabilidad" por enfermería. Rev Latino-am Enfermagem. 2008;16(5). doi: 10.1590/S0104-11692008000500020.
5. Berbesi Fernández DY, Segura Cardona Á. Vulnerability to HIV: A Systematic Review. Investig Andina. 2014;16(28):964-77. doi: 10.33132/01248146.75.
6. De Sousa PK, Miranda K, Franco A. Vulnerabilidade: análise do conceito na prática clínica do enfermeiro em ambulatório de HIV/AIDS. Rev bras enferm. 2011;64(2):381-384. doi: 10.1590/S0034-71672011000200026.
7. Baral SD, Poteat T, Strömdahl S, Wirtz AL, Guadamuz TE, Beyrer C. Worldwide burden of HIV in transgender women: a systematic review and meta-analysis. Lancet Infect Dis. 2013;13(3):214-22. doi: 10.1016/S1473-3099(12)70315-8.
8. United Nations Development Programme. Lost in Transition: Transgender People, Rights and HIV Vulnerability in the Asia-Pacific Region [Internet]. 2012 [citado el 9 de noviembre de 2019]. Disponible en: https://www.undp.org/content/dam/undp/library/hivaids/UNDP_HIV_Transgender_report_Lost_in_Transition_May_2012.pdf.
9. Grupo de Trabajo sobre Tratamientos del VIH. CROI 2016: VIH y transexualidad, una prioridad a la cola de las políticas de prevención y atención [Internet]. [citado el 9 de noviembre de 2019]. Disponible en: http://gttvih.org/actualizate/la_noticia_del_dia/21-03-16.
10. UNAIDS. The gap report transgender people [Internet]. Geneva: Switzerland; 2014 [citado el 9 de noviembre de 2019]. Disponible en: https://www.unaids.org/sites/default/files/media_asset/08_Transgenderpeople.pdf.
11. World Health Organization. Policy brief: Transgender people and HIV [Internet]. Ginebra: WHO; 2015 [citado el 9 de noviembre de 2019]. Disponible en: https://www.who.int/hiv/pub/transgender/transgender-hiv-policy/en/.
12. Silva-Santisteban A, Raymond F, Salazar X, Villayzan J, Leon S, McFarland W, et al. Understanding the HIV/AIDS Epidemic in Transgender Women of Lima, Peru: Results from a Sero-Epidemiologic Study Using Respondent Driven Sampling. AIDS and Behavior. 2012;16(4):872-881. doi: 10.1007/s10461-011-0053-5.
13. Sotelo J. Estudio de seroprevalencia de VIH en personas trans. en: Ministerio de Salud de Argentina. Salud, VIH-sida y sexualidad trans [Internet]. Buenos Aires; 2008 [citado el 9 de noviembre de 2019]. Disponible en: http://new.paho.or/arg/image/KMCA/salud_vih_sida_libro.pdf.
14. Ministerio de Salud y Protección Social, Fondo de Población de las Naciones Unidas. Resultados del estudio comportamiento sexual y prevalencia de infección por VIH en mujeres trans en cuatro ciudades de Colombia, 2012 [Internet]. Bogotá; 2012 [citado el 9 de noviembre de 2019]. Disponible en: http://www.saludcapital.gov.co/DSP/Informes%20Trimestrales%20VIH/2012/Prevalencia%20VIH%20Trans%202012.pdf.
15. Carballo-Diéguez A, Balan I, Marone R, Pando MA, Dolezal C, Barreda V, et al. Use of respondent driven sampling (RDS) generates a very diverse sample of men who have sex with men (MSM) in Buenos Aires, Argentina. PLoS One. 2011;6(11):e27447. doi: 10.1371/journal.pone.0027447.
16. Amon J, Brown T, Hogle J, Macneil J, Magnani R, Mills S, et al. Behavioral Surveillane Surveys (BSS) Guidelines for repeted behavioral Surveys in populations at risk of HIV [Internet]. 2000 [citado el 9 de junio de 2020]. Disponible en: http://www.fhi.org.
17. Poteat T, German D, Flynn C. The conflation of gender and sex: Gaps and opportunities in HIV data among transgender women and MSM. Glob Public Health. 2016;11(7-8):835-48. doi: 10.1080/17441692.2015.1134615.
18. Ayres JR de CM, Paiva V, França I, Gravato N, Lacerda R, Della Negra M, et al. Vulnerability, Human Rights, and Comprehensive Health Care Needs of Young People Living With HIV/AIDS. Am J Public Health. 2006;96(6):1001-6. doi: 10.2105/AJPH.2004.060905.
19. Ayres JRCM, França I, Junqueira G, Saletti HC. O conceito de vulnerabilidade e as práticas em Saúde. Novas perspectivas e desafios. In: Czeresnia D, Machado C, organizadores. Promoção da Saúde: conceitos, reflexões, tendências. 2a ed. Rio de Janeiro: Fiocruz; 2009. p. 121-43.
20. Calazans GJ, Pinheiro TF, Ayres JR. Vulnerabilidade programática e cuidado público: Panorama das políticas de prevenção do HIV e da Aids voltadas para gays e outros HSH no Brasil. Sexualidad, Salud y Sociedad. 2018;(29):263-93. doi: 10.1590/1984-6487.sess.2018.29.13.a.
21. Chazarreta IE. Prostitución y Salud: experiencias invisibilizadas de mujeres y personas trans en Argentina. Rev Reflexiones. 2016;95(1):157. doi: 10.15517/rr.v95i1.27660.
22. Miller WM, Miller WC, Barrington C, Weir SS, Chen SY, Emch ME, et al. Sex work, discrimination, drug use and violence: a pattern for HIV risk among transgender sex workers compared to MSM sex workers and other MSM in Guatemala. Glob Public Health. 2020;15(2):262-74. doi: 10.1080/17441692.2019.1671984.
23. Scheim AI, Bauer GR, Shokoohi M. Drug use among transgender people in Ontario, Canada: Disparities and associations with social exclusion. Addict Behav. 2017;09;72:151-8. doi: 10.1016/j.addbeh.2017.03.022.
24. Santos GM, Rapues J, Wilson EC, Macias O, Packer T, Colfax G, et al. Alcohol and substance use among transgender women in San Francisco: prevalence and association with human immunodeficiency virus infection. Drug Alcohol Rev. 2014;33(3):287-95. doi: 10.1111/dar.12116.
25. Nuttbrock L, Bockting W, Rosenblum A, Hwahng S, Mason M, Macri M, et al. Gender abuse, depressive symptoms, and substance use among transgender women: a 3-year prospective study. Am J Public Health. 2014;104(11):2199-206. doi: 10.2105/AJPH.2014.302106.
26. Fontanari AMV, Pase PF, Churchill S, Soll BMB, Schwarz K, Schneider MA, et al. Dealing with gender-related and general stress: Substance use among Brazilian transgender youth. Addict Behav Rep. 2019;9:100166. doi: 10.1016/j.abrep.2019.100166.
27. Estrada Montoya JH, García Becerra A. Reconfiguraciones de género y vulnerabilidad al VIH/Sida en mujeres transgénero en Colombia. Rev Gerenc y Políticas Salud. 2010;9(18):90-102. doi: 10.11144/Javeriana.rgsp9-18.rgvv.
28. Moriarty KE, Segura ER, Gonzales W, Lake JE, Cabello R, Clark JL. Assessing Sexually Transmitted Infections and HIV Risk Among Transgender Women in Lima, Peru: Beyond Behavior. LGBT Health. 2019;6(7):370-6. doi: 10.1089/lgbt.2018.0087.
29. Foreman M, Lyra P, Breinbauer C. Related Stigma and Discrimination in the Health Sector [Internet]. 2003 [citado el 9 de noviembre de 2019]. Disponible en: https://www.paho.org/hq/dmdocuments/2008/Stigma_report_english.pdf.
30. Dominguez CM, Ramirez SV, Arrivillaga M. Access to Health Servicesfor Transgender Women in the City of Cali, Colombia. MedUNAB. 2017;20(3):296-310. doi: 10.29375/01237047.2404.
Funding: Funding for this study came from the Global Fund to Fight AIDS, Tuberculosis and Malaria, under Grant Agreement No. 216146, signed with Empresa Nacional Promotora de Desarrollo Territorial - Enterritorio, which, in turn, signed a contract with Universidad CES, Medellín, to conduct the study "Sexual behavior and HIV prevalence in transgender women in the cities of Bogotá, Medellín and Santiago de Cali" in 2019. Universidad CES provided funding for the teachers who participated in the study, as principal investigator and co-investigator.
Cite as: Ramos-Jaraba SM, Berbesí-Fernández DY, Bedoya-Mejía S, Molina-Estrada AP, Martínez-Rocha A, Segura-Cardona ÁM. [Factors associated with the perception of hiv vulnerability among transgender women in three Colombian cities]. Rev Peru Med Exp Salud Publica. 2021;38(2):232-9. doi: https://doi.org/10.17843/rpmesp.2021.382.6043.
Correspondence: Dedsy Yajaira Berbesí Fernández; Calle 10A # 22-04, Medellín, Colombia; dberbesi@ces.edu.co
Author contributions: DYBF coordinated the study, participated in its design and execution, and assumes responsibility for all aspects of the manuscript. SMRJ, SBM, APME and AMR coordinated the collection of data in the study cities, participated in the statistical analyses and in writing the article. AMS participated in the statistical analyses of the study and in its design. All authors contributed ideas, reviewed drafts and approved the final version of the article.
Conflicts of interest: The authors declare that there is no conflict of interest.
Received: 06/17/2020
Approved: 03/12/2021
Online: 07/01/2021