Robert Reyna-García
Emilio Aguilar-Huauya
Carlos Santillán-Salas
BRIEF REPORT
Respiratory viruses and clinical- epidemiological characteristics in episodes of acute respiratory infection
Yaquelina Chirinos-Saire ![]() 1, Medical Technologist in Clinical Laboratory and Anatomic Pathology
1, Medical Technologist in Clinical Laboratory and Anatomic Pathology
Robert Reyna-García ![]() 1, Medical Technologist in Clinical
Laboratory and Anatomic Pathology
1, Medical Technologist in Clinical
Laboratory and Anatomic Pathology
Emilio Aguilar-Huauya ![]() 1, Physician specialized in Clinical
Pathology
1, Physician specialized in Clinical
Pathology
Carlos Santillán-Salas ![]() 1, Physician specialized in Infectious
Diseases
1, Physician specialized in Infectious
Diseases
1 Instituto Nacional de Salud del Niño San Borja, Lima, Perú.
ABSTRACT
The aim of the study was to determine the viral frequency and clinical-epidemiological characteristics in the episodes of acute respiratory infection in patients of the Instituto Nacional de Salud del Niño San Borja in Lima, the information of the episodes of patients who required at least one direct Immunofluorescence test from January 1, 2017 to December 31, 2018 was analyzed. 1153 episodes were identified in 707 patients. The median age was 1 year and 55% were male. The viral frequency was 13.4%; respiratory syncytial virus was identified in 10.7% of the episodies. The viral frequency was higher in children under 1 year of age (16.2%); in those with congenital disease respiratory (38.9%) and during the autumn (24.2%). The most common symptoms were cough (70.3%) and fever (53.4%); and the main diagnoses, viral pneumonia (31.8) and bronchiolitis (23.4%). It is concluded that the respiratory viral frequency was related to age, seasonality and pre-existing pathology.
Keywords: Pediatrics; Respiratory Infections; Frequency; Viruses; Fluorescent Antibody Technique, Direct; Peru (source: MeSH NLM).
INTRODUCTION
Acute respiratory infections (ARI) are among the three leading causes of morbidity and mortality in the general population, and the leading cause of mortality in children under five years old, mainly in developing countries (1,2). Viruses are the cause of 80 to 90% of ARI (3), with upper respiratory tract infections being the most frequent. However, pneumonias represent the greatest public health problem (1,4).
In Peru, during 2018 the cumulative incidence rate of ARI episodes was 9,297 per 10,000 children under five years old and the cumulative incidence rate of pneumonia was 100 per 10,000 children under five years old; both with a downward trend in recent years. However, the case fatality rate (1.0 deaths per 100 episodes of pneumonia) has remained constant (5).
Studies conducted abroad show that the frequency of respiratory viruses (RV) in pediatric patients is between 34.1% and 76.7% (6-9), in Peru it has been reported to be between 33.5% and 49.7% (10,11). Currently, in our country there is no detailed information on the frequency of viral infections in children with comorbidities. In addition, there are no studies that compare the frequency of these infections between hospitalized and ambulatory patients, nor their stationary trend that would contribute to establish optimal strategies for surveillance, prevention and control of these infections.
This study aims to describe the frequency of the detection of respiratory viruses and the clinical-epidemiological characteristics of ARI episodes in children attended in the different services of the Instituto Nacional de Salud del Niño San Borja (INSN-SB), a national referral center for the management of pediatric complex diseases, during 2017-2018.
|
KEY MESSAGES |
|
Motivation for the study: In Peru, there are few studies that evaluate the frequency of viral infections in children with comorbidities and their epidemiological and clinical profile. Main findings: Viruses were detected in 13.4% of the episodes of acute respiratory infection; respiratory syncytial virus was the most common pathogen; viral frequency was higher in children younger than 1 year with respiratory congenital diseases and during autumn. Implications: Clinical and epidemiological characterization of patients susceptible to viral respiratory infections will allow improvement of surveillance, prevention and hospital control strategies. |
THE STUDY
Design and study population
We conducted a descriptive, retrospective, cross-sectional study. Laboratorial information was collected from ARI episodes of patients who underwent direct immunofluorescence test (DIF) for RVs, who came from the different services of INSN-SB from January 1, 2017 to December 31, 2018. We included all ARI episodes of patients: a) aged 0 to 18 years, b) inpatients or outpatients, c) with nasopharyngeal swab sampling (NSS). ARI episodes in patients: a) from outside the institution, b) with inadequate sample report were excluded.
An ARI was defined by the presence of one or more symptoms such as cough, rhinorrhea, nasal obstruction, odynophagia, otalgia, wheezing or respiratory distress, with or without fever. An episode of ARI was considered from the first day of symptomatology onset to the fourteenth day.
Procedures
The DIF test for RV was performed as part of the usual institutional care; through the Clinical Pathology Service, samples of NSS were taken, obtained with sterile flocked swabs and placed in a viral transport medium. The samples were transported and stored at a temperature between 2 to 8 °C until processing; following the working protocol of the commercial kit D3 Ultra 8 ™ DFA Respiratory Virus Screening & Identification, for the detection of eight types of RV: adenovirus (ADV), influenza virus A (Flu-A) and B (Flu-B), parainfluenza virus (PIV) 1, 2 and 3, metapneumovirus (hMPV) and respiratory syncytial virus (RSV).
Samples were analyzed with the ZEISS Axio Scope.A1 fluorescence microscope; an adequate sample was considered as the observation of at least 20 columnar epithelial cells in the total number of reading fields. A positive result for RV was defined as the observation of at least two cells with apple green intracellular fluorescence in the total number of reading fields.
The variables in the study were age, sex, year of medical care, type of hospital care, seasonality, baseline disease, current clinical diagnosis, symptomatology, type of RV and viral coinfection.
The data for each episode of ARI were collected from the review of medical records, epidemiological records and the hospital computer system. The information obtained was entered into a spreadsheet in Microsoft Excel 2016.
Statistical analysis
The numerical variable age showed an asymmetric distribution and was summarized with the median and interquartile range (IQR). Categorical variables were presented as absolute and relative frequencies. The data were shown in tables and figures. Comparison for categorical variables was performed with the Chi-square test, and for numerical variables the Mann Whitney U-test was used. A p value <0.05 was considered statistically significant.
Ethical aspects
This study was approved by the INSN-SB Research Ethics Committee. The information collected remained absolutely confidential and was used exclusively for the study.
FINDINGS
During the study period, 1,153 ARI episodes were found in 707 patients who underwent a DIF test for RV (1.6 episodes per patient). Statistical analysis was based on ARI episodes; thus, the frequency of viral detection was 13.4% (154/1153) and it was variable between the two study years and for each type of virus (0.0% to 12.3%). Neither ADV nor Flu-B were detected (Table 1). Of the RV-positive episodes (n=154), the distribution was 7.1% for Flu-A; 7.7% for hMPV; 5.2% for PIV (1-3) and 80% for RSV. No cases of viral coinfection were found.
Table 1. Detection frequency of respiratory viruses in ARI episodes in patients from the Instituto Nacional de Salud del Niño San Borja, 2017-2018.
|
Year |
ARI episodes |
Episodes |
Respiratory viruses |
|||||
|
Flu-A |
hMPV |
PIV-1 |
PIV-2 |
PIV-3 |
RSV |
|||
|
n |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
n (%) |
|
|
2017 |
508 |
52 (10.2) |
4 (0.8) |
0 (0.0) |
1 (0.2) |
2 (0.4) |
1 (0.2) |
44 (8.7) |
|
2018 |
645 |
102 (15.8) |
7 (1.1) |
12 (1.9) |
1 (0.2) |
0 (0.0) |
3 (0.5) |
79 (12.3) |
|
Total |
1,153 |
154 (13.4) |
11 (0.9) |
12 (1.0) |
2 (0.2) |
2 (0.2) |
4 (0.4) |
123 (10.7) |
ARI: acute respiratory infection; RV: respiratory virus; Flu-A: Influenza virus A; hMPV: Metapneumovirus; PIV: Parainfluenza virus; RSV: Respiratory syncytial virus
Of the total ARI episodes, the median age was 1 year (IQR: 0-5); the ages were categorized into four groups, 36.8% of the episodes were recorded in those younger than 1 year, who had a higher viral frequency (16.2%). There were statistically significant differences between the age group and viral frequency (Table 2). Males accounted for 55.9% (n=645) of the episodes with a viral frequency of 12.1% and females (n=519) 14.8%, with no significant differences (p=0.181).
Table 2. Descriptive characteristics in ARI episodes of patients from the Instituto Nacional de Salud del Niño San Borja, according to the detection of respiratory viruses. 2017-2018.
|
Characteristics |
ARI Episodes |
Negative to RV |
Positive to RV (n=154) |
p Value a |
||
|
n |
N |
% |
n |
% |
||
|
Age, median (IQR) |
1 (0-5) |
2 (0-6) |
(0-6) |
1 (0-3) |
(0-3) |
< 0.001b |
|
Age group (years) |
|
|
|
|
|
0.013 |
|
< 1 |
425 |
356 |
83.8 |
69 |
16.2 |
|
|
1-4 |
373 |
319 |
85.5 |
54 |
14.5 |
|
|
5-10 |
271 |
245 |
90.4 |
26 |
9.6 |
|
|
11-18 |
84 |
79 |
94.0 |
5 |
6.0 |
|
|
Sex |
|
|
|
|
|
0.181 |
|
Female |
519 |
442 |
85.2 |
77 |
14.8 |
|
|
Male |
634 |
557 |
87.9 |
77 |
12.1 |
|
|
Year of attention |
|
|
|
|
|
0.006 |
|
2017 |
508 |
456 |
89.8 |
52 |
10.2 |
|
|
2018 |
645 |
543 |
84.2 |
102 |
15.8 |
|
|
Type of attention |
|
|
|
|
|
0.083 |
|
Hospitalization |
837 |
719 |
85.9 |
118 |
14.1 |
|
|
Emergency |
188 |
161 |
85.6 |
27 |
14.4 |
|
|
As outpatients |
128 |
119 |
93.0 |
9 |
7.0 |
|
|
Season |
|
|
|
|
|
< 0.001 |
|
Autumn |
347 |
263 |
75.8 |
84 |
24.2 |
|
|
Summer |
160 |
144 |
90.0 |
16 |
10.0 |
|
|
Winter |
383 |
344 |
89.8 |
39 |
10.2 |
|
|
Spring |
263 |
248 |
94.3 |
15 |
5.7 |
|
|
Baseline disease |
|
|
|
|
|
< 0.001 |
|
Bone marrow aplasia |
48 |
48 |
100.0 |
0 |
0.0 |
|
|
CD. respiratory system |
18 |
11 |
61.1 |
7 |
38.9 |
|
|
CD. circulatory system |
289 |
240 |
83.0 |
49 |
17.0 |
|
|
CD. nervous system |
41 |
34 |
82.9 |
7 |
17.1 |
|
|
CM. digestive tract |
41 |
33 |
80.5 |
8 |
19.5 |
|
|
CM. musculoskeletal system |
14 |
9 |
64.3 |
5 |
35.7 |
|
|
D. digestive system |
17 |
15 |
88.2 |
2 |
11.8 |
|
|
D. nervous system |
44 |
34 |
77.3 |
10 |
22.7 |
|
|
D. respiratory system |
43 |
39 |
90.7 |
4 |
9.3 |
|
|
Hematological neoplasms |
368 |
339 |
92.1 |
29 |
7.9 |
|
|
HCT-SOT |
66 |
59 |
89.4 |
7 |
10.6 |
|
|
Other diseases |
121 |
106 |
87.6 |
15 |
12.4 |
|
|
Previously healthy |
43 |
32 |
74.4 |
11 |
25.6 |
|
ARI: acute respiratory infection; RV: respiratory virus; CD: congenital
disease; CM: congenital malformation; SOT: solid organ transplantation; HCT:
hematopoietic cell transplantation.
a Chi-square test; b Mann Whitney U-test.
The viral frequency in 2017 was 10.2% and in 2018 it was 15.8%, this difference was significant (p=0.006). Of the RV positive episodes, RSV was the most prevalent in both years (84.6% and 77.5%, respectively); the frequency of hMPV was 11.8% in 2018 compared to 0.0% in 2017 (Table 3). Most of the ARI episodes (72.6%) were found to be from the hospitalization area, with a viral frequency of 14.1%, which was similar to those from the Emergency department with 14.4% but different from outpatients, with 7.0% (Table 2).
Table 3. Descriptive characteristics of ARI episodes with viral detection in patients from the Instituto Nacional de Salud del Niño San Borja, according to type of virus. 2017-2018.
|
Characteristics
|
Total RV (+) (n=154) |
Flu- A (n=11) |
hMPV (n=12) |
PIV (1-3) (n=8) |
RSV (n=123) |
||||
|
n |
n % |
% |
n |
% |
n |
% |
n |
% |
|
|
Age, median (IQR) |
|
3 (1-6) |
|
1 (0-1,5) |
|
1,5 (0,5-4,5) |
|
1 (0-3) |
|
|
Age group (years) |
|
|
|
|
|
|
|
|
|
|
< 1 |
69 |
1 |
1.5 |
7 |
10.1 |
2 |
2.9 |
59 |
85.5 |
|
1-4 |
54 |
5 |
9.3 |
4 |
7..4 |
4 |
7.4 |
41 |
75.9 |
|
5-10 |
26 |
4 |
15.3 |
1 |
3.9 |
2 |
7.7 |
19 |
73.1 |
|
11-18 |
5 |
1 |
20.0 |
0 |
0.0 |
0 |
0.0 |
4 |
80.0 |
|
Sex |
|
|
|
|
|
|
|
|
|
|
Female |
77 |
4 |
5.2 |
8 |
10.4 |
3 |
3.9 |
62 |
80.5 |
|
Male |
77 |
7 |
9.1 |
4 |
5.2 |
5 |
6.5 |
61 |
79.2 |
|
Year of attention |
|
|
|
|
|
|
|
|
|
|
2017 |
52 |
4 |
7.7 |
0 |
0.0 |
4 |
7.7 |
44 |
84.6 |
|
2018 |
102 |
7 |
6.9 |
12 |
11.8 |
4 |
3.9 |
79 |
77.5 |
|
Type of attention |
|
|
|
|
|
|
|
|
|
|
Hospitalization |
118 |
5 |
4.2 |
11 |
9.3 |
6 |
5.1 |
96 |
81.4 |
|
Emergency |
27 |
5 |
18.5 |
1 |
3.7 |
2 |
7.4 |
19 |
70.4 |
|
As outpatients |
9 |
1 |
11.1 |
0 |
0.0 |
0 |
0.0 |
8 |
88.9 |
|
Season |
|
|
|
|
|
|
|
|
|
|
Summer |
16 |
3 |
18.7 |
0 |
0.0 |
0 |
0.0 |
13 |
81.3 |
|
Autumn |
84 |
6 |
7.1 |
2 |
2.4 |
0 |
0.0 |
76 |
90.5 |
|
Winter |
39 |
0 |
0.0 |
0 |
0.0 |
7 |
17.9 |
32 |
82.1 |
|
Spring |
15 |
2 |
13.3 |
10 |
66.7 |
1 |
6.7 |
2 |
13.3 |
|
Baseline disease |
|
|
|
|
|
|
|
|
|
|
CD. respiratory system |
7 |
1 |
14.3 |
2 |
28.6 |
0 |
0.0 |
4 |
57.1 |
|
CD. circulatory system |
49 |
4 |
8.2 |
6 |
12.2 |
1 |
2.0 |
38 |
77.6 |
|
CD. nervous system |
7 |
0 |
0.0 |
1 |
14.3 |
0 |
0.0 |
6 |
85.7 |
|
CM. digestive tract |
8 |
0 |
0.0 |
2 |
25.0 |
1 |
12.5 |
5 |
62.5 |
|
CM. musculoskeletal system |
5 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
5 |
100.0 |
|
D. nervous system |
10 |
0 |
0.0 |
0 |
0.0 |
2 |
20.0 |
8 |
80.0 |
|
Hematological neoplasms |
29 |
3 |
10.3 |
0 |
0.0 |
3 |
10.3 |
23 |
79.3 |
|
HCT-SOT |
7 |
1 |
14.3 |
0 |
0.0 |
1 |
14.3 |
5 |
71.4 |
|
Other diseases |
21 |
2 |
9.5 |
1 |
4.8 |
0 |
0.0 |
18 |
85.7 |
|
Previously healthy |
11 |
0 |
0.0 |
0 |
0.0 |
0 |
0.0 |
11 |
100.0 |
|
Clinical diagnosis |
|
|
|
|
|
|
|
|
|
|
Rhinopharyngitis |
8 |
0 |
0.0 |
1 |
12.5 |
1 |
12.5 |
6 |
75.0 |
|
Influenza |
5 |
0 |
0.0 |
0 |
0.0 |
1 |
20.0 |
4 |
80.0 |
|
Asthmatic crisis |
3 |
1 |
33.0 |
0 |
0.0 |
0 |
0.0 |
2 |
66.7 |
|
Bronchiolitis |
36 |
3 |
8.3 |
0 |
0.0 |
1 |
2.8 |
32 |
88.9 |
|
Viral pneumonia |
49 |
1 |
2.0 |
7 |
14.3 |
2 |
4.1 |
39 |
79.6 |
|
Unspecified ARI |
53 |
6 |
11.3 |
4 |
7.5 |
3 |
5.7 |
40 |
75.5 |
ARI: acute respiratory infection; RV: respiratory virus; CD: congenital disease; CM: congenital malformation; SOT: solid organ transplantation; HCT: hematopoietic cell transplantation.
ARI episodes were more frequent during the winter and autumn seasons; the highest viral frequency occurred in autumn (24.2%), there were significant differences between seasons (p<0.001). Between the months of February and April 2017, and May and July 2018, the highest viral frequency was recorded between 20.7% to 25.5% and 41.6% to 21.6%, respectively (Figure 1). During summer, autumn and winter, RSV was the main pathogen; while in spring it was hMPV (Table 3).
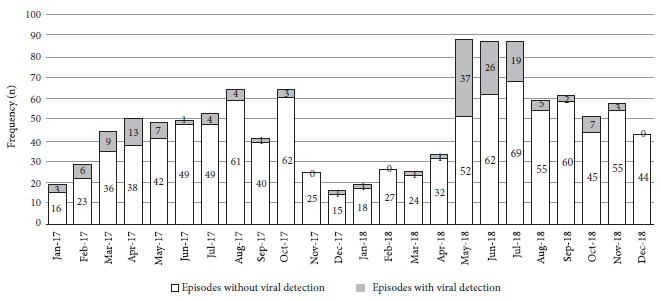
Figure 1. Distribution of the 1,153 ARI episodes during the months of 2017 and 2018, according to viral detection.
Of the total number of ARI episodes, 96.3% had an underlying condition, hematologic neoplasm (HN) and congenital disease of the circulatory system (CD-CS) were the most frequent with 31.9% and 25.1%, respectively. Viral frequency was higher in cases with congenital disease of the respiratory system (CD-RS) (38.9%) and congenital malformation of the musculoskeletal system (CM-MS) (35.7%), there were significant differences between pre-existing conditions (p<0.001) (Table 2).
Among the episodes with viral detection, the most frequent clinical diagnoses were viral pneumonia (31.8%) and bronchiolitis (23.4%). In episodes with bronchiolitis, RSV was identified in 88.9%; in those with pneumonia, RSV and hMPV were in 79.6% and 14.3%, respectively (Table 3). The most frequent clinical manifestations in 148/154 episodes were cough (70.3%), fever (53.4%), rhinorrhea (52.7%), dyspnea (51.3%) and wheezing (50.7%).
DISCUSSION
In this study, the viral detection frequency was 13.4% among all ARI episodes identified. Previously published studies reported a viral prevalence between 11.9% to 49.7% in pediatric patients without reported comorbidities and with viral detection by DIF (6,7,10,11). This study found that viral infections were more frequent in children under 1 year of age and in children under 5 years of age; for the latter age group, different studies reported a viral frequency between 14.8% to 40% (7,10,12); this percentage variation could be due to a heterogeneous child population, presence or absence of underlying diseases, different geographic settings or different surveillance and control measures in health care facilities.
The viral frequency obtained from the hospitalization area was similar to that from the emergency department, and higher than in the outpatients; we observed that hospitalization and emergency patients presented similar characteristics regarding the age group (those under 3 years of age represented 64%) and regarding comorbidity, mainly cases of CD-CS. Meanwhile, outpatients were mainly 5 to 10 years old and with HN or HCT. Viral detection was highest during autumn and lowest during spring, with Flu-A and RSV being mainly detected during autumn, PIV during winter and hMPV during spring; these data are consistent with other studies from South America (8,10,13).
Viral infections, mainly those caused by RSV, can increase the risk of morbimortality in patients with congenital heart disease, HN, chronic respiratory diseases, congenital malformations of the respiratory system and prematurity. Cardiopathic children under 2 years of age have a higher risk of malnutrition, which predisposes them to of viral infections (14).
The main pathogen identified in our study was RSV, with a high detection rate in cases with CD-RS (4/18) and with CM-MS (5/14); however, we consider that a larger sample of those diseases should be needed for a better analysis. The finding of RSV in cases with CD-CS (13.1%) was similar to that reported previously (15,16); while regarding HN, the viral frequency (6.3%) was lower compared to other studies (7% to 42%) (17); no viral detection was registered in the neonatal intensive care unit, compared to a study that reported 47% of viral infection (18).
This study was carried out using a screening panel for the main viruses causing ARI, a considerably large number of ARI episodes, including all pediatric ages, inpatient and outpatient cases, with different pre-existing diseases and over a 2-year period, allowing the evaluation of seasonal trends.
The limitations of the study include: selection biases, probably the sickest group of patients was chosen for the medical consultation, there was no standardized criterion to determine which patients underwent the DIF test for RV. Regarding detection biases, it is possible that patients with earlier infections were the only ones that could have been identified, while those with infections with an evolution of more than seven days could not be identified. The results cannot be extrapolated to the community. The time of evolution of the disease could not be determined because the information on the date of onset of symptoms was incomplete in some cases. Other frequent RV, such as rhinovirus and coronavirus (detection by RT-PCR) were not evaluated, which probably led to a lower viral frequency.
In conclusion, the frequency of RV was related to age, seasonality and pre-existing disease, and RSV was found to be the main pathogen. This study contributes to a better understanding of the characterization of ARI in pediatric patients, especially in those with pre-existing disease.
We consider it is convenient to carry out studies to characterize viral respiratory infections in pediatric patients with different comorbidities, including the detection of other frequent viruses, taking into account the time of evolution of the disease. Likewise, studies should be carried out to identify the risk factors associated with viral respiratory infection in children with pre-existing pathologies.
Acknowledgments:
The authors express their gratitude to Dr. María Medina P. for reviewing the project and final report, Dr. Emiliana Rizo-Patrón T. for advice on the statistical analysis, Drs. Carla Méndez-Chacón R. and Carlos Jamieson V. for reviewing the project, Lab. Tec. Claudio Vega L. for his support in obtaining the data, and to Eng. Jimmy Vásquez R. and his team for allowing the review of the clinical histories.
Authors’ contributions: YCS participated in the conception and design of the article; analysis and interpretation of data, writing of the article; critical revision of the article. RRG participated in the conception and design of the article; data collection. EAH participated in the conception and design of the study. CSS participated in the analysis and interpretation of data and critical revision of the article. All authors participated in the approval of the final version of the article.
Conflicts of interest: None of the authors have conflicts of interest.
Funding: This research was self-funded.
REFERENCES
1. Foro de las Sociedades Respiratorias Internacionales. El impacto global de la Enfermedad respiratoria - segunda edición [Internet]. Mexico: Asociación Latinoamericana de Tórax; 2017 p. 9, 18-21 [citado el 21 de enero de 2019] Disponible en: https://www.who.int/gard/publications/The_Global_Impact_of_Respiratory_Disease_ES.pdf.
2. Organización Mundial de la Salud. Neumonía [Internet]. Ginebra: OMS; 2020 [citado 9 de noviembre de 2020]. Disponible en: https://www.who.int/es/news-room/fact-sheets/detail/pneumonia#:~:text=La%20neumon%C3%ADa%20es%20la%20principal,a%C3%B1os%20en%20todo%20el%20mundo.
3. Juy E, Céspedes E, Rubal A, Maza A, Terán C. Morbilidad por infecciones respiratorias agudas en menores de 5 años. MEDISAN 2014;18(11):1490-8.
4. European Respiratory Society. Acute lower respiratory infections [Internet]. European Lung White Book [citado 8 de noviembre de 2020]. Disponible en: https://www.erswhitebook.org/chapters/acute-lower-respiratory-infections/.
5. Ministerio de Salud. Boletín epidemiológico del Perú, volumen 27 - SE 52 [Internet]. Lima: Dirección General de Epidemiología, MINSA; 2018 [citado 19 de noviembre de 2020]. Disponible en: https://www.dge.gob.pe/portal/docs/vigilancia/boletines/2018/52.pdf.
6. Ge X, Han Z, Chen H, Cheng J, Gao M, Sun H. Characterization of acute respiratory infections among 340 infants in Wuxi, Jiangsu Province. Ann Transl Med. 2015;3(18):264. doi: 10.3978/j.issn.2305-5839.2015.10.23.
7. Spano A, Lamantía E, Terán L, Daniele R, Sanchez L, Cabral M. Inmunofluorescencia indirecta versus Reacción de cadena de la polimerasa en tiempo real para la detección de Virus respiratorios. Rev Bioanálisis. 2019; 15(91):8-18.
8. Marcone DN, Carballal G, Ricarte C, Echavarría M. Diagnóstico de virus respiratorios utilizando un sistema automatizado de PCR múltiples (FilmArray) y su comparación con métodos convencionales. Rev Argent Microbiol. 2015;47(1):29-35. doi: 10.1016/j.ram.2014.12.003.
9. Wong-Chew RM, Espinoza MA, Taboada B, Aponte FE, Arias-Ortiz MA, Monge-Martínez J, et al. Prevalence of respiratory virus in symptomatic children in private physician office settings in five communities of the state of Veracruz, Mexico. BMC Res Notes. 2015;8:261. doi: 10.1186/s13104-015-1239-0.
10. Del Valle J, Cornejo-Tapia A, Weilg P, Verne E, Nazario‐Fuertes R, Ugarte C, et al. Incidence of respiratory viruses in peruvian children with acute respiratory infections. J Med Virol. 2015;87(6):917-24. doi: 10.1002/jmv.24159.
11. Mezarina-Esquivel H, Bada-Mancilla C, Castañeda-Campozano R. Identificación viral en pacientes hospitalizados por infecciones respiratorias bajas, en menores de 5 años, en el hospital de emergencias pediatricas. Lima - Perú, 2014. Rev Peru Investig Materno Perinat. 2017;6(2):9-12. doi: 10.33421/inmp.201790.
12. Wang H, Zheng Y, Deng J, Wang W, Liu P, Yang F, et al. Prevalence of respiratory viruses among children Hospitalized from respiratory infections in Shenzhen, China. Virol J. 2016;13(39). doi: 10.1186/s12985-016-0493-7.
13. Becerra M, Fiestas V, Tantaleán J, Mallma G, Alvarado M, Gutiérrez V, et al. Etiología viral de las infecciones respiratorias agudas graves en una unidad de cuidados intensivos pediátricos. Rev Peru Med Exp Salud Publica. 2019;36(2):231-8. doi: 10.17843/rpmesp.2019.362.4081.
14. Medrano López C, García-Guereta Silva L. Infecciones respiratorias y cardiopatías congénitas: dos estaciones del estudio CIVIC. An Pediatría. 2007;67(4):329-36. doi: 10.1016/S1695-4033(07)70650-1.
15. Sahan Y, Kılıçoğlu E, Tutar Z. Evaluation of Children with Congenital Heart Disease Hospitalized with the Diagnosis of Lower Respiratory Tract Infection. J Pediatr Res. 2018;5(1):32-6. doi: 10.4274/jpr.90532.
16. Resch B, Kurath-Koller S, Hahn J, Raith W, Köstenberger M, Gamillscheg A. Respiratory syncytial virus-associated hospitalizations over three consecutive seasons in children with congenital heart disease. Eur J Clin Microbiol Infect Dis. 2016;35(7):1165-9. doi: 10.1007/s10096-016-2649-1.
17. Saavedra-Lozano J, Garrido C, Catalán P, González F. Niños con cáncer e infección viral respiratoria: epidemiología, diagnóstico y posibles tratamientos. Enfermedades Infecc Microbiol Clínica. 2011;29(1):40-51. doi: 10.1016/j.eimc.2010.04.011.
18. Moreno Parejo C, Morillo García A, Lozano Domínguez C, Carreño Ochoa C, Aznar Martín J, Conde Herrera M. Brote por virus respiratorio sincitial en la Unidad de Neonatología de un hospital de tercer nivel. An Pediatría. 2016;85(3):119-27. doi: 10.1016/j.anpedi.2015.10.002.
Correspondence: Yaquelina Chirinos-Saire; Servicio de Patología Clínica, INSN-SB, Av. Agustín de la Rosa Toro 1399, Urb. Jacaranda II - San Borja, Lima, Perú; yaquy_cs@hotmail.com
Cite as: Chirinos-Saire Y, Reyna-García R, Aguilar-Huauya E, Santillán-Salas C. Virus respiratorios y características clínico-epidemiológicas en los episodios de infección respiratoria aguda. Rev Peru Med Exp Salud Publica. 2021;38(1):101-7. doi: https://doi.org/10.17843/rpmesp.2021.381.6346.
Received: 18/08/2020
Approved: 02/12/2020
Online: 01/02/2021