Maria J. Pons
Susan Mosquito
Theresa J. Ochoa
Yolanda Sáenz
BRIEF REPORT
Characterization of Escherichia coli D7111 producing the β-LACTAMASE TEM-176
Joaquim Ruiz ![]() 1,
PhD in Biology
1,
PhD in Biology
Maria J. Pons ![]() 1, PhD in Biology
1, PhD in Biology
Susan Mosquito ![]() 2, PhD in Biology
2, PhD in Biology
Theresa J. Ochoa ![]() 2,3, Pediatric infectologist physician, PhD in
Medicine
2,3, Pediatric infectologist physician, PhD in
Medicine
Yolanda Sáenz ![]() 4, PhD in Biochemistry and Molecular and Cellular
Biology
4, PhD in Biochemistry and Molecular and Cellular
Biology
1 Laboratorio de
Genética Molecular y Bioquímica, Universidad Científica del Sur, Lima, Perú.
2 Instituto de Medicina Tropical «Alexander von Humboldt»,
Universidad Peruana Cayetano Heredia, Lima, Perú.
3 School of Public Health, University of Texas Health Science
Center at Houston, Houston, Estados Unidos.
4 Área de Microbiología Molecular, Centro de Investigación
Biomédica de La Rioja, Logroño, España.
ABSTRACT
The present report is the original description of blaTEM-176. The mechanisms of resistance to antimicrobial agents were determined in an enterotoxigenic Escherichia coli, determining the susceptibility to 22 antimicrobials classified in 15 different groups by agar diffusion and establishing the phylogenetic group, mechanisms of resistance and presence of Class 1 and 2 integrons. Integrons and β-lactam resistance genes were sequenced. The isolate, belonging to phylogenetic group A, showed the presence of resistance or diminished susceptibility to a ampicillin, amoxicillin plus clavulanic acid, nalidíxic acid, ciprofloxacin, streptomycin, kanamycin, tetracycline, trimethoprim, sulfisoxazole, cotrimoxazole, azithromycin and nitrofurantoin, carrying blaTEM, aadA1/2, aphA1, sul3, tet(A) and a Class 2 integron containing a dfrA1 gene. Quinolone resistance was related to the substitution Ser83Ala. The TEM sequencing showed the presence of the new substitution Ala222Val, which led to the description of the new β-lactamase blaTEM-176.
Keywords: Ampicillin; Amoxicillin-Clavulanic Acid; beta-Lactamases; Antibacterial Drug Resistance; Enterotoxigenic Escherichia coli; Molecular Epidemiology; Integrons (source: MeSH NLM).
INTRODUCTION
The β-lactam family is one of the most widely used antibiotic families worldwide, both in human and veterinary healthcare. However, the emergence of microorganisms resistant to these antibiotics compromises their usefulness. Thus, in some areas, including different regions of Peru, the levels of resistance to the oldest β-lactams, such as ampicillin, border or exceed 90% (1,2). Meanwhile, resistance levels to more modern β-lactams, such as 3rd and 4th generation cephalosporins, are around 50% (3).
In gram-negative bacteria, resistance to β-lactams is mainly associated with the production of β-lactamases. Among these, the TEM-type β-lactamases are the most frequent, and have been widely reported in Peru (2,3), although in most cases only their presence has been determined, without developing sequencing studies to determine variants.
In this context, in 2007, during a study on childhood diarrhea and antimicrobial resistance carried out in Lima, a diarrheagenic (enterotoxigenic) strain of Escherichia coli D7111 (1) was isolated, which was molecularly characterized by identifying the blaTEM gene variant. Therefore, this report aims to molecularly characterize the E. coli D7111 strain including the original description of the blaTEM-176 gene.
|
KEY MESSAGES |
|
Motivation for the study: Although several studies in Peru have established the presence of blaTEM, there is a lack of data on the circulating variants. Main findings: An Escherichia coli blaTEM gene was sequenced, presenting a single variation, leading to the Ala222Val change, with respect to TEM-1. At the time of the study (2010) the sequence obtained had not been described, and was given the name of blaTEM-176. Implications: The detection of a new β-lactamase, shows the presence of resistance genes not described in the area, suggesting that whole genes should be sequenced when possible. |
THE STUDY
The E. coli D7111 strain was isolated during a passive prospective cohort study conducted in peri-urban areas of southern Lima that included 1,034 children between 2 and 12 months of age (1).
Sensitivity to 22 antimicrobials categorized into 15 groups was obtained by agar diffusion (4). Thus, we determined resistance to penicillins (ampicillin), penicillins + β-lactamase inhibitors (amoxicillin plus clavulanic acid [AMC]), cephamycins (cefoxitin), extended-spectrum cephalosporins (cefotaxime, ceftazidime, cefepime), monobactams (aztreonam), carbapenems (imipenem), aminoglycosides (amikacin, gentamicin, kanamycin), streptomycins (streptomycin), amphenicols (chloramphenicol), quinolones (nalidixic acid), fluoroquinolones (ciprofloxacin, norfloxacin), folate inhibitors (trimethoprim, cotrimoxazole), macrolides (azithromycin), tetracyclines (tetracycline), phosphonic acids (fosfomycin), nitrofurans (nitrofurantoin) and sulfonamides (sulfisoxazole). The results were interpreted according to the 2010 Clinical and Laboratory Standards Institute (CLSI) guidelines (4).
The presence of extended-spectrum β-lactamases (ESBL) was analyzed with the double-disk synergy test (3), while presence of plasmid AmpC (pAmpC) was determined by comparison of cefoxitin disk inhibition diameters in the presence or absence of 200 µg cloxacillin (5).
The presence of β-lactamases CARB type, OXA-1-like, OXA-2-like, OXA-5-like, SHV and TEM was determined by PCR (Polymerase Chain Reaction) (Table 1). Positive products were recovered, purified and sent to Macrogen (Seoul, South Korea) for two-way sequencing.
Table 1. Primers used in this study
|
Gene |
Primer 1 |
Primer 2 |
bp |
°C |
Ref |
|
blaTEM |
ATTCTTGAAGACGAAAGGGC |
ACGCTCAGTGGAACGAAAAC |
1,150 |
60 |
3 |
|
blaSHV |
ATGCGTTATATTCGCCTGTG |
TTAGCGTTGCCAGTGCTCG |
841 |
55 |
3 |
|
blaCARB |
AATGGCAATCAGCGCTTC |
GGGGCTTGATGCTCACT |
586 |
56 |
3 |
|
blaOXA-1-LIKE |
ACCAGATTCAACTTTCAA |
TCTTGGCTTTTATGCTTG |
598 |
55 |
3 |
|
blaOXA-2-LIKE |
CGATAGTTGTGGCAGACGAA |
CCACTCAACCCATCCTACCC |
550 |
55 |
3 |
|
blaOXA-5-LIKE |
TATATTCCAGCATCAACATT |
ATGATGCCCTCACTTGCCAT |
605 |
55 |
3 |
|
gyrA |
AAATCTGCCCGTGTCGTTGGT |
GCCATACCTACGGCGATACC |
343 |
55 |
3 |
|
parC |
AAACCTGTTCAGCGCCGCATT |
GTGGTGCCGTTAAGCAAA |
395 |
59 |
3 |
|
aphA1 |
ATGGGCTCGCGATAATGTC |
CTCACCGAGGCAGTTCCAT |
600 |
50 |
6 |
|
aphA2 |
GAACAAGATGGATTGCACGC |
GCTCTTCAGCAATATCACGG |
680 |
50 |
6 |
|
aadA1, aadA2 |
GCAGCGCAATGACATTCTTG |
ATCCTTCGGCGCGATTTTG |
282 |
60 |
6 |
|
tet(A) |
GTAATTCTGAGCACTGTCGC |
CTGCCTGGACAACATTGCTT |
937 |
62 |
6 |
|
tet(B) |
CTCAGTATTCCAAGCCTTTG |
CTAAGCACTTGTCTCCTGTT |
416 |
57 |
6 |
|
dfrA1,dfr5, dfr15, dfr15b, dfr16, dfr16b |
GTGAAACTATCACTAATGG |
TTAACCCTTTTGCCAGATTT |
474 |
55 |
6 |
|
dfrA6,dfr14 |
GAGCAGCTICTITTIAAAGC |
TTAGCCCTTTIICCAATTTT |
393 |
60 |
6 |
|
dfrA7, dfr17 |
TTGAAAATTTCATTGATT |
TTAGCCTTTTTTCCAAATCT |
474 |
55 |
6 |
|
dfrA12, dfr13 |
GGTGSGCAGAAGATTTTTCGC |
TGGGAAGAAGGCGTCACCCTC |
319 |
60 |
6 |
|
sul1 |
TGGTGACGGTGTTCGGCATTC |
GCGAGGGTTTCCGAGAAGGTG |
789 |
63 |
6 |
|
sul2 |
CGGCATCGTCAACATAACC |
GTGTGCGGATGAAGTCAG |
722 |
50 |
6 |
|
sul3 |
CATTCTAGAAAACAGTCGTAGTTCG |
CATCTGCAGCTAACCTAGGGCTTTGGA |
990 |
51 |
6 |
|
VR1 |
GGCATCCAAGCAGCAAG |
AAGCAGACTTGACCTGA |
Var. |
55 |
6 |
|
VR2 |
CGGGATCCCGGACGGCATGCACGATTTGTA |
GATGCCATCGCAAGTACGAG |
Var. |
60 |
6 |
|
chuA |
GACGAACCAACGGTCAGGAT |
TGCCGCCAGTACCAAAGACA |
279 |
59 |
7 |
|
yjaA |
TGAAGTGTCAGGAGACGCTG |
ATGGAGAATGCGTTCCTCAAC- |
211 |
59 |
7 |
|
tspE4C2 |
GAGTAATGTCGGGGCATTCA |
CGCGCCAACAAAGTATTACG |
152 |
59 |
7 |
bp: amplicon size in base pairs; °C: banding temperature; Ref: Reference; VR: Variable Region (1 - of Class 1 integrons; 2 - of Class 2 integrons); Var: Variable.
Phylogenetic groups were established by PCR (simultaneous amplification of chuA, yjaA and tspE4C2). We also established the presence of aadA1/2, aphA1 (aph(3')-Ia) and aphA2 (aph(3' )-IIa) genes involved in resistance to streptomycins and aminoglycosides; tet(A) and tet(B) involved in resistance to tetracyclines; dfrA1, dfrA5, dfrA6, dfrA7, dfrA12, dfrA13, dfrA14, dfrA15, dfrA15b, dfrA16, dfrA16b, dfrA17 related to the development of resistance to trimethoprim and sul1, sul2 and sul3 which cause resistance to sulfonamides. Additionally, the presence of Class 1 and Class 2 integrons was determined by PCR, and the quinolone resistance determinant region of the gyrA and parC genes was amplified (Table 1). In the case of the dfr genes, the variant was identified by RFLP (Restriction Fragment Length Polymorphism) of the amplicons obtained according to the methodology previously described (6,7). Mutations in gyrA and parC as well as integron-positive products were characterized by sequencing.
Information on the reference sequences (DNA/ Amino Acids) of the resistance genes considered in this study (as well as others) can be found at https://www.ncbi.nlm.nih.gov/refseq/.
The original study was approved by the Ethics Committee of the Institute for Nutritional Research under code 246- 2006/CEI-IIN.
FINDINGS
Strain E. coli D7111, identified as belonging to phylogroup A, showed resistance to ampicillin, AMC, azithromycin, cotrimoxazole, kanamycin, sulfisoxazole, tetracycline, trimethoprim and nalidixic acid, as well as intermediate sensitivity to streptomycin, nitrofurantoin and ciprofloxacin (Table 2). In the case of azithromycin, the inhibition halo was <6 mm, so that even in the absence of the cut-off point established by CLSI, we classified it as resistant.
Table 2. Resistance profile and underlying mechanisms.
|
Antimicrobial |
Sensitivity |
Mechanism |
|
Ampicillin |
R |
TEM-176 |
|
AMC |
R |
TEM-176? |
|
Cefoxitin |
S |
--- |
|
Cefotaxime |
S |
--- |
|
Ceftazidime |
S |
--- |
|
Cefepime |
S |
--- |
|
Aztreonam |
S |
--- |
|
Imipenem |
S |
|
|
Nalidixic Acid |
R |
Ser83Ala (GyrA) |
|
Ciprofloxacin |
I |
Ser83Ala (GyrA) |
|
Norfloxacin |
S |
Ser83Ala (GyrA) |
|
Amikacin |
S |
--- |
|
Gentamicin |
S |
--- |
|
Kanamycin |
R |
APH(3’)-Ia |
|
Streptomycin |
I |
ANT(3’’)-I |
|
Azithromycin |
R |
ND |
|
Chloramphenicol |
S |
|
|
Trimethoprim |
R |
DfrA1 |
|
Sulfisoxazole |
R |
Sul3 |
|
Cotrimoxazole |
R |
DfrA1 + Sul3 |
|
Tetracycline |
R |
Tet(A) |
|
Nitrofurantoin |
I |
ND |
|
Fosfomycin |
S |
|
AMC: Amoxicillin plus clavulanic acid; S: Susceptible; I: Intermediate; R: Resistant; ND: Not determined; ?: Not established.
The phenotypic study of β-lactamases was negative for both ESBL and pAmpC, with blaTEM being the only β-lactamase coding gene amplified. The sequencing result showed the presence of a nucleotide-level difference (A665T) regarding the blaTEM-1 sequence, leading to the amino acidic change Ala222Val. After comparing the amino acid sequence with those described to date, it was verified as novel and was submitted to the corresponding repository (www.lahey.com, currently transferred to the National Center for Biotechnology Information - NCBI - https://www.ncbi.nlm.nih.gov/pathogens/submit-beta-lactamase/), being confirmed as a new TEM variant, and received the name TEM-176 (Figure 1). Consequently, the sequence was reported to GenBank, and is accessible under the codes: GU550123 - Original DNA Sequence; NG_050215 - Reference DNA Sequence; Reference Protein Sequence WP_038976851.
In lowercase letters is the sequence of a 1043 bp DNA fragment containing the blaTEM-176 gene (GenBank: GU550123), above it is annotated in uppercase letters the amino acidic sequence of TEM-176. In bold and highlighted in yellow are the differences with respect to TEM-1 (GenBank: NG_050145), amino acidic at the top, nucleotidic at the bottom.
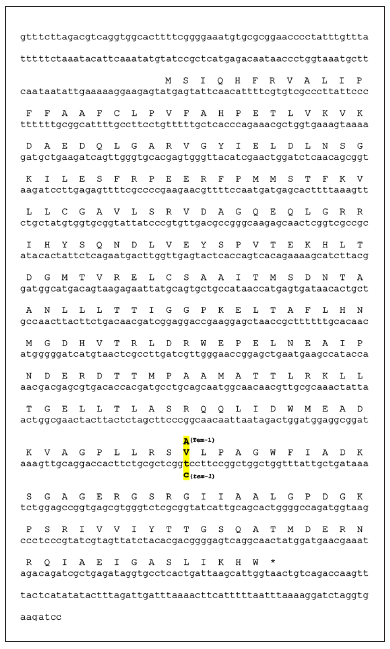
Figure 1. blaTEM-176 gene sequence.
Additionally, E. coli strain D7111 presented the genes aadA1/2, aphA1 (coding for the aminoglycoside-modifying enzyme, APH(3')-Ia), tet(A), dfrA1 and sul3 as well as the amino acidic change Ser83Ala in GyrA. The integron study showed the presence of a class 2 integron, of approximately 800 bp, containing the dfrA1 gene cassette (Table 2).
DISCUSSION
This study reports the presence of a TEM variant that, at the time of the study, had not been identified and, after being submitted to the entity who oversees nomenclature, was given the name TEM-176.
The β-lactamase family of TEM-type β-lactamases was initially described in 1965 (8), currently counting 190 variants sequenced and present at https://www.ncbi.nlm.nih.gov/pathogens/refgene/#gene_family:(blaTEM) ranging from TEM-1 to TEM-242 (note the absence in the NCBI database of TEM-type β-lactamases with assigned numbering).
TEM-176 differs by only one amino acid from TEM-1. Although apparently insignificant, differences of one amino acid may imply differences in the spectrum of activity (both on existing β-lactams and on β-lactams to be designed at later times after their description). Likewise, these differences may have evolutionary implications, since the acquisition of a point mutation could make TEM-176 evolve more easily to other TEM variants, including ESBL, as would be the case of TEM-147 (Reference Protein Sequence: WP_063864859), which has only one amino acid difference with respect to TEM-176, Arg162His, in addition to the presence of Val222.
After its detection in strain D7111 and its inclusion in the nomenclature, TEM-176 has been described on several occasions. Thus, GenBank (https://www.ncbi.nlm.nih.gov/ipg/WP_038976851.1) reports its presence in E. coli (29 strains), Salmonella enterica (61 strains, belonging to frequent serotypes such as Typhimurium, Enteritidis or Hadar, or infrequent ones such as Brancaster or Schwarzengrund), Klebsiella pneumoniae (2 strains), Citrobacter amalonaticus (2 strains), Citrobacter portucalensis (1 strain) and Vibrio parahaemolyticus (2 strains), being in most cases detected during genomic sequencing studies.
The presence of this (or other) blaTEM variants has probably gone unnoticed in numerous studies, given the need to sequence the blaTEM amplicon in order to make the correct identification. The fact that it does not affect 3rd and 4th generation cephalosporins may also have contributed to this. Nevertheless, since its description and introduction in GenBank on January 31, 2010, blaTEM-176 has been reported in microorganisms isolated from samples of different origins (e.g. human, animal or food), and from several geographic locations, such as Austria, Australia, Ecuador, Singapore or Tanzania, thus showing worldwide dissemination (9-13).
Although there is scarce data on its genomic location, in some cases its presence has been proven in plasmids of the IncX group (10,11), such as pSGMCR103 (a plasmid of the IncX1 group), which, among other resistance determinants, in addition to blaTEM-176, carries the mcr-5.1 gene (11).
In addition, its presence has been detected in metagenomic studies carried out in Peru (14). This fact is interesting, since it would appear that despite the scarcity of studies aimed at sequencing β-lactamase type TEM in Peru, the presence of TEM-176 has been described by different authors independently in the country, suggesting that it could be relatively frequent in the area.
The fact that strain D7111 is resistant to AMC, together with the non-detection of other β-lactamases, opens the door to the possibility that this β-lactamase inhibitor does not completely inhibit TEM-176, which would allow this β-lactamase to be categorized as IRT (Inhibitor Resistant TEM). However, this aspect should be specifically and unequivocally verified, since unidentified β-lactamases could coexist, just as it has been found that overexpression of β-lactamases of the TEM type, such as TEM-1, can lead to decreased sensitivity or resistance to AMC (15).
Strain D7111 also presented other resistance determinants, such as the aphA1 gene, underlying the detection of resistance to kanamycin (16). APH(3')-Ia has been previously described in numerous microorganisms, including all gram-negative bacteria of the ESKAPE group (Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa and Enterobacter spp.) as well as other microorganisms causing different diseases such as Escherichia coli or Salmonella spp. (https://card.mcmaster.ca/ontology/39041). However, to our knowledge, this is the first description of this enzyme in Peru. The ubiquity of APH(3')-Ia together with the high levels of kanamycin resistance detected in clinical isolates in Peru makes this finding not surprising. Another aminoglycoside-modifying enzyme-encoding gene, an aadA-type gene, was also detected. The aadA genes encode nucleotidyltransferases inactivating streptomycin and spectinomycin (16), and are widely disseminated worldwide, although unlike in this case, they are often associated with integrons, both Class 1 and Class 2 (http://integrall.bio.ua.pt/).
Consistent with what has been described in the literature, the Ala83 substitution in GyrA was considered to be the cause of resistance to nalidixic acid (17,18). This amino acid change is associated with less alteration of the hydrophobicity patterns of GyrA than other amino acid changes at the same position such as Ser83Leu or Ser83Val, and therefore is usually associated with lower levels of resistance (17,18).
In addition to tetracycline, Tet(A) has been associated with slight increases in resistance to tigecycline, moreover, the development during treatments of new allelic variants (amino acidic change Ser251Ala) capable of conferring minimum inhibitory concentration levels of 32 mg/L has been observed (19).
Integrons are mobilizable genetic structures, although not mobile per se, which are characterized by having a 5' end consisting of a gene coding for an integrase, a series of gene cassettes coding for genes of various kinds and a 3' end that varies among the different types of integrons, but that is highly conserved (20). Integrons are classified according to the integrase gene, with classes 1 and 2 being the most common, usually carrying resistance genes (20), and they receive a specific numbering based on their content (type and order) of gene cassettes (http://integrall.bio.ua.pt/). The integron detected in this strain is a class 2 integron containing the dfrA1 gene, concordant with the In2-2 integron (http://integrall.bio.ua.pt/). This dfrA1 gene underlies resistance to trimethoprim, and together with the sul3 gene, responsible for resistance to sulfisoxazole, underlies resistance to co-trimoxazole.
The complete study of this strain and the sequencing of blaTEM-176 was developed in 2010, so the elapsed time is the major limitation for this study, creating a paradox in which there are publications where the presence of blaTEM-176 is reported prior to the original report of this β-lactamase. Likewise, it remains to evaluate the real effect of AMC and the potential as IRT of TEM-176, which should be done by cloning this gene in a cloning vector that does not contain another β-lactamase, in order to avoid erroneous interpretations due to the added action of both enzymes.
In conclusion, the mechanisms of antimicrobial resistance present in strain D7111 are characterized, and reporting the original description of TEM-176. Likewise, the detection of TEM-176 in subsequent studies developed in Peru is emphasized, suggesting the stable presence of this resistance determinant in the area.
Author contributions: All authors participated in the conception and design of the article. MJP and SM participated in experimental development; data analysis and interpretation. JR and MJP participated in the drafting of the article. All authors critically reviewed the article, approved the final version and assume responsibility for the contents of the manuscript.
Conflicts of interest: The authors declare no conflicts of interest.
Funding: JR was funded by the Fondo Nacional de Desarrollo Científico, Tecnológico y de Innovación Tecnológica (FONDECYT-Peru) under the "Proyecto de Mejoramiento y Ampliación de los Servicios del Sistema Nacional de Ciencia, Tecnología e Innovación Tecnológica" (contract number 08-2019-FONDECYT-BM-INC-INV).
REFERENCES
1. Ochoa TJ, Ruiz J, Molina M, del Valle LJ, Vargas M, Gil AI, et al. High frequency of antimicrobial drug resistance of diarrheagenic Escherichia coli in infants in Peru. Am J Trop Med Hyg. 2009;81:296-301.
2. Granda A, Riveros M, Martínez-Puchol S, Ocampo K, Laureano-Adame L, Corujo A, et al. Presence of extended-spectrum β-lactamase, CTX-M-65, in Salmonella enterica serovar Infantis isolated from children with diarrhea in Lima, Peru. J Pediatric Infect. Dis. 2019;14:194-200. doi: 10.1055/s-0039-1685502.
3. Palma N, Pons MJ, Gomes C, Mateu J, Riveros M, García W, et al. Resistance to quinolones, cephalosporins and macrolides in Escherichia coli causing bacteraemia in Peruvian children. J Global Antimicrob Resist. 2017;11:28-33. doi: 10.1016/j.jgar.2017.06.011.
4. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, Twentieth Information Supplement M100S-16. Wayne: CLSI; 2010.
5. de Toro M, Seral C, Rojo-Bezares B, Torres C, Castillo FJ, Sáenz Y. Resistencia a antibióticos y factores de virulencia en aislados clínicos de Salmonella enterica. Enferm Infecc Microbiol Clin. 2014;32:4-10. doi: 10.1016/j.eimc.2013.03.006.
6. Sáenz Y, Briñas L, Domínguez E, Ruiz J, Zarazaga M, Vila J, et al. Mechanisms of resistance in multiple-antibiotic-resistant Escherichia coli strains of human, animal, and food origins. Antimicrob Agents Chemother. 2004;48:3996-4001. doi: 10.1128/AAC.48.10.3996-4001.2004.
7. Clermont O, Bonacorsi S, Bingen E. Rapid and simple determination of the Escherichia coli phylogenetic group. Appl Environ Microbiol. 2000;66:4555-8. doi: 10.1128/aem.66.10.4555-4558.2000.
8. Datta N, Kontomichalou P. Penicillinase synthesis controlled by infectious R factors in Enterobacteriaceae. Nature. 1965;208:239-41. doi: 10.1038/208239a0.
9. Desvars-Larrive A, Ruppitsch W, Lepuschitz S, Szostak MP, Spergser J, Feßler AT, et al. Urban brown rats (Rattus norvegicus) as possible source of multidrug-resistant Enterobacteriaceae and meticillin-resistant Staphylococcus spp., Vienna, Austria, 2016 and 2017. Euro Surveill. 2019;24:1900149. doi: 10.2807/1560-7917.ES.2019.24.32.1900149.
10. Dobiasova H, Dolejska M. Prevalence and diversity of IncX plasmids carrying fluoroquinolone and β-lactam resistance genes in Escherichia coli originating from diverse sources and geographical areas. J Antimicrob Chemother. 2016;71:2118-24. doi: 10.1093/jac/dkw144.
11. Guo S, Tay MYF, Thu AK, Seow KLG, Zhong Y, Ng LC, et al. Conjugative IncX1 plasmid harboring colistin resistance gene mcr-5.1 in Escherichia coli isolated from chicken rice retailed in Singapore. Antimicrob Agents Chemother. 2019;63:e01043-19. doi: 10.1128/AAC.01043-19.
12. Mshana SE, Hain T, Domann E, Lyamuya EF, Chakraborty T, Imirzalioglu C. Predominance of Klebsiella pneumoniae ST14 carrying CTX-M-15 causing neonatal sepsis in Tanzania. BMC Infect Dis. 2013;13:466. doi: 10.1186/1471-2334-13-466.
13. Vinueza-Burgos C, Ortega-Paredes D, Narváez C, De Zutter L, Zurita J. Characterization of cefotaxime resistant Escherichia coli isolated from broiler farms in Ecuador. PLoS One. 2019;14:e0207567. doi: 10.1371/journal.pone.0207567.
14. Pehrsson EC, Tsukayama P, Patel S, Mejía-Bautista M, Sosa-Soto G, Navarrete KM, et al. Interconnected microbiomes and resistomes in low-income human habitats. Nature. 2016;533:212-6. doi: 10.1038/nature17672.
15. Stapleton P, Wu PJ, King A, Shannon K,French G, Philips I. Incidence and mechanisms of resistance to the combination of amoxicillin and clavulanate in Escherichia coli. Antimicrob Agents Chemother. 1995;39: 2478-83.
16. Goñi MP, Agudo MC, Gómez-Lus R. Antibiòtics aminoglicòsids. Treb Soc Cat Biol. 2004;55:107-19.
17. Ruiz J. Mechanisms of resistance to quinolones: target alterations, decreased accumulation and DNA gyrase protection. J Antimicrob Chemother. 2003;51:1109-17. doi: 10.1093/jac/dkg222.
18. Ruiz J. Quinolones: acció i resistencia. Treb Soc Cat Biol. 2004; 55: 131-8.
19. Du X, He F, Shi Q, Zhao F, Xu J, Fu Y, et al. The rapid emergence of tigecycline resistance in blaKPC-2 harboring Klebsiella pneumoniae, as mediated in vivo by mutation in tetA during tigecycline treatment. Front Microbiol. 2018;9:648. doi: 10.3389/fmicb.2018.00648.
20. Li Y, Yang L, Fu J, Yan M, Chen D, Zhang L. Genotyping and high flux sequencing of the bacterial pathogenic elements - integrons. Microb Pathog. 2018;116:22-5. doi: 10.1016/j.micpath.2017.12.073.
Correspondence: Joaquim Ruiz, Laboratorio de Genética Molecular y Bioquímica, Universidad Científica del Sur, Panamericana Sur Km 19, Lima, Peru; joruiz.trabajo@gmail.com
Cite as: Ruiz J, Pons MJ, Mosquito S, Ochoa TJ, Sáenz Y. Characterization of Escherichia coli D7111 producing the β-LACTAMASE TEM-176. Rev Peru Med Exp Salud Publica. 2021;38(1):130-35. doi: https://doi.org/10.17843/rpmesp.2021.381.5108.
Received: 18/08/2020
Approved: 06/01/2021
Online: 03/02/2021