Manuel Chu
Jesús Guzmán
Denis Castillo
Michel Sauvain
Original article
Diagnostic performance of the culture and susceptibility of Helicobacter pylori in peruvian patients: results from a sentinel laboratory
Maricruz Olano ![]() 1,2, Degree in Biology
1,2, Degree in Biology
Manuel Chu ![]() 1,2, Biologist, Master in Biochemistry and Molecular Biology
1,2, Biologist, Master in Biochemistry and Molecular Biology
Jesús Guzmán ![]() 1,2, Pharmaceutical chemist, Master in Biochemistry and Molecular Biology
1,2, Pharmaceutical chemist, Master in Biochemistry and Molecular Biology
Denis Castillo ![]() 1,2, Biologist, Master in Biochemistry and Molecular Biology
1,2, Biologist, Master in Biochemistry and Molecular Biology
Michel Sauvain ![]() 1,2,Pharmaceutical chemist, PhD in Pharmacochemistry
1,2,Pharmaceutical chemist, PhD in Pharmacochemistry
1 Laboratorio Mixto Internacional Andino Amazónico de Química de la Vida, Universidad Peruana Cayetano Heredia. Lima, Peru.
2 Laboratorio Centinela de Helicobacter pylori, Instituto de Medicina Tropical Alexander von Humboldt, Universidad Peruana Cayetano Heredia, Lima, Peru.
ABSTRACT
Objective: To analyze the antimicrobial susceptibility of Helicobacter pylori to 5 reference antibiotics, in a population of 500 dyspeptic patients from the Gastroenterology Service of the Cayetano Heredia Hospital (n = 419) and the Cayetano Heredia Clinic (n = 81) in Lima, Peru.
Materials and methods: Gastric biopsies were collected from 500 patients diagnosed with dyspepsia. From these biopsies, 273 H. pylori strains were isolated and cultured to confirm H. pylori infection by histological and culture diagnosis. Finally, antimicrobial susceptibility was analyzed using the broth microdilution method, and the resistance profiles of each antimicrobial and multi-resistance patterns were evaluated by statistical analysis.
Results: The diagnosis of H. pylori infection by culture, compared to histological testing, reported a sensitivity of 83.8%, a specificity of 89.9% and an area under the curve (AUC) of 0.87 (95% CI: 0.84 to 0.90). The frequency of infection in the gastroenterology services of the Cayetano Heredia Hospital and Clinic was 56.6% (237/419) and 44.4% (36/81), respectively. An increase in antimicrobial resistance to Amoxicillin (45.1% / 29.6%), Levofloxacin (71.8%/ 74.1%) and Metronidazole (69.8% / 63.0%) was found in the Hospital and the Clinic, respectively. Multiple resistance patterns showed that the most frequent resistance (double and triple) was to Levofloxacin, Metronidazole and Amoxicillin.
Conclusions: The antimicrobial resistance of H. pylori has increased compared to that reported in previous years. Furthermore, H. pylori multiple resistance presents high frequencies in infected patients. The broth microdilution method could be implemented in different hospitals in Peru as a surveillance tool for H. pylori antimicrobial resistance.
Keywords: Helicobacter pylori; Prevalence; Diagnosis; Drug Resistance; Drug Resistance Multiple.
INTRODUCTION
Helicobacter pylori (H. pylori) is a human pathogen and the causative agent of gastroduodenal diseases associated with stomach tissue malignancy (1). It is estimated that, worldwide, the prevalence of this infection exceeds 50% and reaches 64% of the population in Latin America. This prevalence varies widely among countries; in Peru it is 45%, and in populations with low socioeconomic status and difficult access to healthcare services it can be up to 80% (2).
In clinical practice, the detection of H. pylori is carried out by invasive or non-invasive methods. Non-invasive methods, such as the exhaled urea test or the fecal antigen test, are of interest and show sensitivity and specificity above 95%. On the other hand, invasive methods, based on biopsy, facilitate the subsequent typing of the pathogen. According to Frías (3), the invasive method based on gastric biopsy as a routine strategy allows histological identification of the bacterium and its subsequent isolation for analysis of epidemiological interest (4).
Treatment of H. pylori infection is based on the use of standard triple therapy, which uses the antimicrobials clarithromycin plus amoxicillin or metronidazole plus a proton pump inhibitor. The use of second-line antimicrobials, such as levofloxacin and tetracycline, is recommended in the case of therapeutic failure against the infection. However, the increase in antimicrobial resistance is a global public health problem and limits the usefulness of treatment due to loss of efficacy as a consequence of the use of inadequate doses, lack of adherence to treatment, high gastric acidity, high bacterial load and, as the main factor, the appearance of antibiotic-resistant strains (5).
This study evaluated the susceptibility to 5 standard antimicrobials used in the first and second line of treatment against H. pylori infection, such as amoxicillin, clarithromycin, levofloxacin, metronidazole and tetracycline, in order to determine the resistance frequency. In addition, the receiver operating characteristic (ROC) was analyzed to evaluate the performance of culture versus histological diagnosis, and the concordance between them was determined using the kappa index.
|
KEY MESSAGES |
|
Motivation for the study: In Peru, antimicrobial resistance rates to Helicobacter pylori have increased. Information regarding reference drugs is still scarce due to the difficulty of culture, which limits antimicrobial susceptibility testing. Main findings: A high percentage of H. pylori infection was found. Antimicrobial resistance, mainly to amoxicillin and levofloxacin, has increased. Implications: The use of the broth microdilution technique could be implemented in different hospitals in Peru as a tool for surveillance of H. pylori resistance to antimicrobials. |
MATERIALS AND MEHODS
Study design and population
We carried out a descriptive cross-sectional study, it included 500 volunteers with dyspepsia symptoms who had not received treatment for H. pylori infection three months prior to enrollment and who had indication for biopsy by endoscopy at the Gastroenterology Service of the Cayetano Heredia Hospital (CHH) (n = 419) and the Cayetano Heredia Clinic (CHC) (n = 81), Lima, Peru, between March 2016 and August 2017. Participants voluntarily signed the informed consent for the study, which was approved by the Institutional Ethics Committee for Humans of the Universidad Peruana Cayetano Heredia (Statement 59026- 15 with enrollment code 63157). Each sample and strain were coded to maintain confidentiality. Due to the different socioeconomic origin of the patients, the analysis was independent for each center (6).
For this study, H. pylori infection was diagnosed using the invasive endoscopic method and gastric biopsies were taken from dyspeptic patients for isolation of H. pylori strains.
Bacteria and culture conditions
The isolation of H. pylori strains began with the collection of gastric mucosal biopsies by endoscopy. The biopsies were transported independently in BHI broth (BD®) supplemented with 10% glycerol (Sigma-Aldrich®) at 4 °C. Gastric mucosa samples were disaggregated using 40 µm cell disaggregation meshes (BD®); the process was carried out under cold chain conditions in a time interval of less than three hours and then, an aliquot of the homogenate was taken for blood culture on agar (BHI agar [BD®]) with 10% defibrinated lamb blood, amphotericin B (Sigma-Alcrich®) and Skirrow selective supplement (Oxoid®) at 37 °C under microaerobiosis conditions (5% O2 and 10% CO2) for 3-5 days (7).
Histological and culture diagnosis
Histological analysis was conducted by staining biopsies with hematoxylin-eosin and observing H. pylori bacteria at 1000× under a light microscope. Diagnosis by culture was made by identification of colonies on blood agar plates according to their appearance, Gram staining, and biochemical oxidase, catalase, and urease tests. A patient was considered infected when positive for at least one diagnostic strategy. Both strategies were compared and histological diagnosis was considered the gold standard in order to estimate the performance of diagnosis by culture (7,8).
Evaluation of antimicrobial susceptibility
The minimum inhibitory concentration (MIC) was determined by using the broth microdilution strategy, and the reference strain of Helicobacter pylori ATCC 43504 was used as a control. For each isolate, an inoculum equivalent to the 2.0 McFarland standard (1×107 to 1×108 CFU/mL) was prepared in BHI broth (BD®) with 10% fetal bovine serum (SigmaAldrich®) and 1% nutrient supplement for fastidious microorganisms (Isovitalex®). Amoxicillin, clarithromycin, levofloxacin, metronidazole and tetracycline (SigmaAldrich®) were added to the medium at initial concentrations of 0.48 µg/mL, 2 µg/mL, 4 µg/mL, 64 µg/mL and 4 µg/mL respectively, from which four serial dilutions were made. Then, incubation was conducted at 37 °C under microaerobic conditions for 72 hours. The isolated strains were considered resistant based on the cut-off points recommended by the European Committee on Antibiograms (EUCAST) (9). The assays were carried out in triplicate and we considered the MIC profiles recommended by the Clinical and Laboratory Standards Institute (CLSI) (10) for the reference strain ATCC 43504.
Statistical analysis
A descriptive analysis of the frequency of cases was carried out to determine the resistance profile of each antimicrobial and multidrug-resistance patterns. Sensitivity, specificity, positive predictive value, negative predictive value and area under the curve (AUC) were calculated by ROC analysis, considering the histological test as the gold standard, and the Kappa index was used to determine concordance between both strategies. Susceptibility analysis was reported in frequencies. The MIC50 and MIC90 were calculated using Probit regression analysis. The analysis was carried out at a 95% confidence level and a significance level of 5%. Data were entered into an Excel 2016 spreadsheet and analyzed with the statistical package Stata/SE 15.1.
RESULTS
A total of 500 samples from patients with dyspepsia were analyzed. Diagnosis by culture, compared to histological testing, showed a sensitivity of 83.8%, a specificity of 89.9% and an AUC of 0.87 (95% CI: 0.84 to 0.90) (Figure 1).
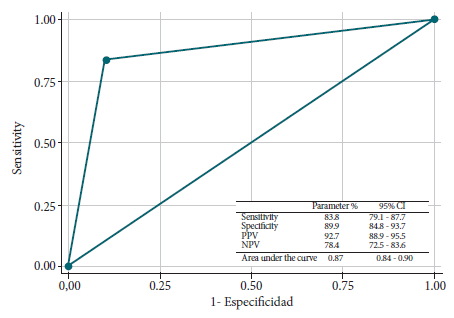
Figure 1. Performance of the diagnostic test by culture compared to histology as a reference test.
The frequencies of H. pylori infection in the gastroenterology services of the Cayetano Heredia Hospital and Clinic were 56.6% and 44.4%, respectively, and were obtained by microbiological culture diagnosis. Meanwhile, the infection frequencies were 61.1% in the Hospital and 56.8% in the Clinic by histological diagnosis. Concordance between the diagnosis by microbiological culture and histology, determined by the kappa index (K), was 0.71 for the Hospital and 0.76 for the Cayetano Heredia Clinic (Table 1).
Table 1. Distribution of cases with dyspepsia diagnosed according to diagnostic strategy by culture and histology.
|
Location |
H. pylori diagnostic |
Kappa (95% CI) |
p-Value |
|
|
Histology (%) |
Culture (%) |
|||
|
Hospital |
61.1 (256/419) |
56.6 (237/419) |
0.71 (0.64-0.79) |
0.001 |
|
(n=419) |
||||
|
Clinic |
56.8 (46/81) |
44.4 (36/81) |
0.76 (0.57-0.94) |
0.001 |
|
(n=81) |
||||
The susceptibility evaluation in the Gastroenterology Service of the Cayetano Heredia Hospital, carried out using the broth microdilution test, showed antibiotic resistance frequencies for H. pylori of 45.1% for amoxicillin, 33.3% for clarithromycin, 71.8% for levofloxacin, 69.8% for metronidazole, and 9.1% for tetracycline. At the Cayetano Heredia Clinic, the frequency of antibiotic resistance was 29.6% for amoxicillin, 48.2% for clarithromycin, 74.1% for levofloxacin and 63.0% for metronidazole. The frequency of antibiotic resistance to tetracycline in the Gastroenterology Service of the Cayetano Heredia Clinic was 0%. The minimum 50% inhibitory concentration (MIC50) of H. pylori strains for amoxicillin was twice as high in the Hospital (0.27 µg/ml) as that observed in the Cayetano Heredia Clinic (0.13µg/ml) (Table 2).
Table 2. Susceptibility patterns of H. pylori isolates according to the reference antimicrobial used.
|
Variable |
A |
C |
L |
M |
T |
|
H. pylori ATCC 43504 (µg/ml) |
0.015-0.125 |
0.015-0.125 |
0.064-0.5 |
64-256 |
0.12-1 |
|
Cut-off point (EUCAST) - Resistance (µg/ml) |
>0.12 |
>0.5 |
>1 |
>8 |
>1 |
|
Resistance frequency - Hospital (%) |
45.1 |
33.3 |
71.8 |
69.8 |
9.1 |
|
MIC50 |
0.27 |
<0.25 |
2.40 |
17.12 |
<0.25 |
|
MIC90 |
0.91 |
3.11 |
4.62 |
35.55 |
1.80 |
|
Resistance frequency - Clinic (%) |
29.6 |
48.2 |
74.1 |
63.0 |
0.0 |
|
MIC50 |
0.13 |
<0.25 |
3.41 |
22.35 |
0.25 |
|
MIC90 |
0.71 |
2.45 |
7.39 |
59.73 |
0.40 |
N: 273 isolated strains of Helicobacter pylori (Hospital: 237, Clinic: 36)
MIC50: Minimum concentration that inhibits 50% of H. pylori strains. MIC90: Minimum concentration that inhibits 90% of H. pylori strains.
A: amoxicillin; C: clarithromycin; L: levofloxacin; M: metronidazole; T: tetracycline.
Of the 179 positive cases for H. pylori from Hospital Cayetano Heredia and the 27 positive cases from the Cayetano Heredia Clinic, we found that the resistance to two antimicrobials was 21.8% (39/179) and 33.3% (9/27), respectively. In addition, we observed that triple resistance was the most frequent (29.1%) among the isolates from the Cayetano Heredia Hospital, meanwhile double resistance was the most frequent (33.3%) in isolates from the Cayetano Heredia Clinic. The most frequent quadruple resistance pattern in both centers involved the antimicrobials amoxicillin, clarithromycin, levofloxacin and metronidazole with percentages of 11.7% and 11.1%, for the Hospital and the Clinic respectively. The Clinic did not have any isolates with quintuple resistance, meanwhile a frequency of 5.6% was found among the isolates from the Hospital for this type of resistance (Table 3).
Table 3. Multiple resistance patterns of H. pylori isolates for each reference antimicrobial.
|
Location |
Double resistance |
Triple resistance |
Quadruple resistance |
Resistance to all antibiotics |
|||||||||
|
AL |
AM |
CL |
CM |
LM |
ACL |
ACM |
ALM |
CLM |
CLT LMT |
ACLM |
ALMT |
ACLMT |
|
|
Hospital n (%) |
6 (3.4) |
7 (3.9) |
3 (1.7) |
2 (1.1) |
21 (11.7) |
3 (1.7) |
4 (2.2) |
26 (14.5) |
15 (8.4) |
1 (0.6) 3 (3.7) |
21 (11.7) |
2 (1.1) |
10 (5.6) |
|
Total n (%) |
39 (21.8) |
|
|
|
|
52 (29.1) |
|
|
|
|
23 (12.8) |
|
10 (5.6) |
|
Clinic n (%) |
1 (3.7) |
-- |
1 (3.7) |
-- |
7 (25.9) |
1 (3.7) |
1 (3.7) |
1 (3.7) |
5 (18.5) |
-- -- |
3 (11.1) |
-- |
-- |
|
Total n (%) |
9 (33.3) |
|
|
|
|
8 (29.6) |
|
|
|
|
3 (11.1) |
|
|
N: 206 multidrug-resistant Helicobacter pylori strains (Hospital: 179, Clinic: 27).
A: amoxicillin; C: clarithromycin; L: levofloxacin; M: metronidazole; T: tetracycline.
DISCUSSION
The diagnosis of H. pylori infection by microbiological culture is considered a more specific detection method that allows the development of various strategies, such as genotypic classification of the microorganism, evaluation of the activity and toxicity of new and usual drugs, virulence profile surveillance of strains from patients and determination of antimicrobial resistance, as well as the implementation of biobanks to carry out future epidemiological studies (11). This study found that the microbiological culture has moderate concordance with routine detection tests, and observed statistically significant kappa indexes of K=0.71 for the Hospital and K=0.76 for the Cayetano Heredia Clinic when compared with the histological test defined as gold standard.
The frequencies of H. pylori infection were 56.6% for the Cayetano Heredia Hospital and 44.4% for the Cayetano Heredia Clinic. These infection frequency patterns are comparable to what was reported in 2017 for the Hospital (58.9%) and in 2015 for Cayetano Heredia Clinic (46.3%) (7,12,15). At the moment, there are still insufficient studies on H. pylori infection frequencies in the Peru.
In Peru, there are reports on the H. pylori resistance to antibiotics, using the methods of microdilution in egg yolk agar, disk diffusion, agar dilution and epsilon test or E-test (13-15). In 2019, Guzman et al, reported antimicrobial resistance rates using the broth microdilution method for the first time in H. pylori strains isolated from dyspeptic patients enrolled in 2015 for the same private health center. The percentage of H. pylori infection was 46.3% and the percentage of resistance to clarithromycin was 52.3%, thus obtaining contrasting results with those described in our study.
The complex molecular mechanisms of antibiotic resistance in H. pylori limit the use of molecular strategies for typing the reference set of antimicrobials used for eradication, making classical microbiological strategies suitable for antimicrobial susceptibility assessment. In our study, antimicrobial susceptibility assessment showed an increase in resistance frequencies of metronidazole 69.8% (CHH), 63% (CHC) with respect to 61.8% and 29.6% of 2017 and 2019, respectively(15,12); of levofloxacin, 71.8% (CHH) and 74.1% (CHC) exceed the resistance rate of 36.8%, 53.9% and 45.5% of 2011, 2013 and 2015, respectively (16,15,12); and of clarithromycin, 33.3% (CHH) and 48.2% (CHC), our results were contrasting with what was reported in 2017 by Boehnke (15), Lima, Peru.
Regarding the analysis of resistance to amoxicillin, we observed an increase in both medical centers (45.1% for the Hospital and 29.6% for the Clinic) compared to studies by other authors such as Boehnke et al, (32.9% in the Hospital) (15) and Guzman et al, (4.6% in the Clinic) (12). The increase in the resistance frequency may be influenced by the increase in the consumption of these drugs in recent years, reaching 70% with respect to other antimicrobials, and consumption without medical prescription (17).
In our study, 69.3% and 74.1% of the isolates from dyspeptic patients from the Hospital and Cayetano Heredia Clinic presented a multidrug-resistant pattern, respectively. Triple resistance (29.1%) and double resistance (33.3%) were the most frequent for Cayetano Heredia Hospital and Cayetano Heredia Clinic, respectively. Only the Hospital had multidrug resistance to all 5 antimicrobials (5.6%). In addition, we observed that the least affected drug was tetracycline. This multidrug resistance is higher compared to what was found in other countries. In Mexico, double resistance (30.7%) and triple resistance (8.7%) among H. pylori isolates has been reported (18). Similarly, multiple resistant strains were detected in Asian (8.3%), American (15%) and European (8.9%) patients (19,20).
Currently, triple therapy, which includes two antibiotics and a proton pump inhibitor, is used as a treatment for H. pylori infection. The most commonly used antibiotics are clarithromycin, metronidazole, amoxicillin and levofloxacin, the latter as a second-line or rescue drug. In our study, we observed that the multi-resistance patterns are evenly distributed for both centers, with a higher frequency of the metronidazole and levofloxacin double resistance pattern of 11.7% and 25.9% for isolates from Cayetano Heredia Hospital and Cayetano Heredia Clinic, respectively. In addition, the most frequent triple resistance patterns involved both metronidazole and levofloxacin and added amoxicillin among Hospital isolates (14.5%), while in the Clinic the triple pattern added clarithromycin to the metronidazole and levofloxacin association with a triple resistance rate of 18.5%. The highest frequency of cases with quadruple resistance in both the Hospital and the Clinic considered the drugs amoxicillin, clarithromycin, levofloxacin and metronidazole. Despite the low frequency of the multiple resistance pattern, amoxicillin, clarithromycin and tetracycline, with a proton pump inhibitor could be suggested as combination therapy for the treatment of H. pylori infection in our population. However, the high frequency of independently detected resistance to amoxicillin and clarithromycin (45.1% and 33.3%, respectively) should be considered.
Results of antimicrobial susceptibility, using the broth microdilution method, were obtained based on the determination of MIC and cut-off points reported by EUCAST to indicate whether the H. pylori strain is sensitive or resistant to the antibiotics under study. Further studies are needed to validate the broth microdilution method as a standard method for the evaluation of H. pylori resistance to antimicrobials. It is also important to carry out longitudinal studies for the evaluation of the efficacy of current treatments against the infection and, in this way, to propose routine surveillance of H. pylori antimicrobial resistance in the country.
In conclusion, the frequency of antibiotic resistance for H. pylori at the Cayetano Heredia Hospital was 45.1% for amoxicillin, 33.3% for clarithromycin, 71.8% for levofloxacin, 69.8% for metronidazole and 9.1% for tetracycline. At the Cayetano Heredia Clinic, we observed resistance frequencies of 29.6% to amoxicillin, 48.2% to clarithromycin, 74.1% to levofloxacin and 63.0% to metronidazole.
Acknowledgments: We thank Dr. Jorge Luis Huerta-Mercado Tenorio and the staff of the Gastroenterology Services of the Cayetano Heredia Hospital and Clinic, especially nurse Nátaly Ojeda Oyague, for their interest and dedication to our research.
Funding: FONDECYT and CIENCIACTIVA, through financial support received under the project "Sentinel laboratory prototype to monitor Helicobacter pylori resistance to antibiotics in Peru". Project 1172015 executed at the Alexander von Humboldt Institute of Tropical Medicine - UPCH with the Research Institute for Development IRD-France.
Author contributions: JG, DC, and MS conceived and designed the study; JG, MC, and MO collected the data; JG and MO processed, analyzed, and interpreted the data; JG and MO drafted the article; DC and MS critically reviewed the article. All authors approved the final version.
Conflicts of interest: The authors declare that they have no conflicts of interest.
REFERENCES
1. Dubois A. Spiral bacteria in the human stomach: the gastric helicobacters. Emerg Infect Dis. 1995;1(3):79-85. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2626874/.
2. Sjomina O, Pavlova J, Niv Y, Leja M. Epidemiology of Helicobacter pylori infection. Helicobacter. 2018;23 Suppl 1: e12514. doi: 10.1111/hel.12514.
3. Frías-Ordoñez JS, Otero-Regino W. Aspectos prácticos en métodos diagnósticos para la infección por Helicobacter pylori: una revisión narrativa. Rev Gastroenterol Perú. 2017; 37(3): 246-253.
4. Lash JG, Genta RM. Adherence to the Sydney System guidelines increases the detection of Helicobacter gastritis and intestinal metaplasia in 400738 sets of gastric biopsies. Aliment Pharmacol Ther. 2013 Aug;38(4):424-31. doi: 10.1111/apt.12383.
5. Malfertheiner P, Megraud F, O’Morain CA. on behalf of the European Helicobacter and Microbiota Study Group and Consensus panel, et al. Management of Helicobacter pylori infection—the Maastricht V/Florence Consensus Report Gut 2017;66:6-30. doi: 10.1136/gutjnl-2016-312288.
6. Aliaga RJ, Cedron CH, Pinto VJ. Comparación de prevalencia de infección por Helicobacter pylori en pacientes con dispepsia entre dos instituciones de diferentes estratos socioeconómicos en el periodo 2017-2018. Rev. Gastroenterol Perú. 2019;39(3):211-214.
7. Guzmán J, Castillo D, Ojeda M, Sauvain M. Susceptibilidad antimicrobiana y mutaciones en el gen ARNr 23s de Helicobacter pylori en pacientes dispépticos. Rev Peru Med Exp Salud Pública. 2019;36(2):270-4. doi: http://dx.doi.org/10.17843/rpmesp.2019.362.3901.
8. Ndip RN, MacKay WG, Farthing MJ, Weaver LT. Culturing Helicobacter pylori from clinical specimens: review of microbiologic methods. J Pediatr Gastroenterol Nutr. 2003;36(5):616-22. doi: 10.1097/00005176-200305000-00005.
9. European Committee on Antimicrobial Susceptibility Testing. Breakpoint tables for interpretation of MICs and zone diameters. Version 9.0, 2019 [Internet]. Basilea: EUCAST; 2019 [Citado el 20 de octubre de 2018] Disponible en: http://www.eucast.org/fileadmin/src/media/PDFs/EUCAST_files/Breakpoint_tables/v_9.0_Breakpoint_Tables.pdf.
10. Clinical and Laboratory Standars Institute. Methods for antimicrobial dilution and disk susceptibility testing of infrequently isolated or fastidious bacteria; Approved Guideline-Second edition. Wayne, PA: CLSI; 2010. [Citado 20 octubre de 2018] Disponible en: https://clsi.org/media/1450/m45ed3_sample.pdf.
11. Frías-Ordoñez JS, Otero-Regino W. Aspectos prácticos en métodos diagnósticos para la infección por Helicobacter pylori: una revisión narrativa. Rev Gastroenterol Perú. 2017; 37(3): 246-253.
12. Guzmán J, Castillo D, Ojeda M, Sauvain M. Susceptibilidad antimicrobiana y mutaciones en el gen ARNr 23s de Helicobacter pylori en pacientes dispépticos. Rev Peru Med Exp Salud Pública. 2019;36(2):270-4. doi: 10.17843/rpmesp.2019.362.3901.
13. Vásquez A, Valdez Y, Gilman RH, McDonald JJ, Westblom TU, Berg D,et al. Metronidazole and clarithromycin resistance in Helicobacter pylori determined by measuring MICs of antimicrobial agents in color indicator egg yolk agar in a miniwell format. The Gastrointestinal Physiology Working Group of Universidad Peruana Cayetano Heredia and the Johns Hopkins University. J Clin Microbiol. 1996;34(5):1232–1234. doi: 10.1128/jcm.34.5.1232-1234.1996.
14. Alarcón T, Domingo D, López-Brea M. Los problemas de resistencia a antibióticos con Helicobacter pylori. Int J Antimicrob Agents. 1999; 12(1):19-26. doi: 10.1016/s0924-8579(99)00051-5.
15. Boehnke KF, Valdivieso M, Bussalleu A, Sexton R, Thompson KC, Osorio S, et al. Antibiotic resistance among Helicobacter pylori clinical isolates in Lima, Peru. Infect Drug Resist. 2017; 10:85-90. doi: 10.2147/IDR.S123798.
16. Mochizuki H, Noriega AP. Determinación de la susceptibilidad de cepas de Helicobacter pylori a Levofloxacino en formato pequeño y método de difusión en disco usando Agar yema de huevo. Rev Gastroenterol Perú. 2011;31(3):224-9.
17. Megraud F, Coenen S, Versporten A, Kist M, Lopez-Brea M, Hirschl AM, et al. Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut. 2013;62(1):34-42. doi: 10.1136/gutjnl-2012-302254.
18. Torres J, Camorlinga-Ponce M, Perez-Perez G, Medrazo-De la Garza A, Dehesa M, Gonzalez-Valencia G, et al. Increasing multidrug resistance in Helicobacter pylori strains isolated from children and adults in Mexico. J Clin Microbiol. 2001; 39:2677–80. doi: 10.1128/JCM.39.7.2677-2680.2001.
19. De Francesco V, Floriana G, Cesare H, Gianpiero M, Lucy V, Carmine P, et al. Worldwide H. pylori antibiotic resistance: a systematic review. J Gastrointestin Liver Dis. 2010;19(4):409–14.
20. Kouitcheu Mabeku LB, Eyoum Bille B, Tepap Zemnou C. Broad spectrum resistance in Helicobacter pylori isolated from gastric biopsies of patients with dyspepsia in Cameroon and efflux-mediated multiresistance detection in MDR isolates. BMC Infect Dis 19, 880 2019. doi: 10.1186/s12879-019-4536-8.
Cite as: Olano M, Chu M, Guzmán J, Castillo D, Sauvain M. Diagnostic Performance of the Culture and Susceptibility of Helicobacter pylori in Peruvian Patients: Results from a Sentinel Laboratory. Rev Peru Med Exp Salud Publica. 2021;38(3):406-11. doi: https://doi.org/10.17843/rpmesp.2021.383.7256
Correspondence: Michel Henri Sauvain; michel.sauvain@ird.fr
Received: 02/02/2021
Approved: 08/09/2021
Online: 31/09/2021