Nelson E. Arias-Ortiz
Walter A. Arboleda-Ruiz
Original article
Incidence, mortality and survival of endometrial cancer in Manizales, Colombia 2003-2017
María C. Montoya-González ![]() 1, Physician, Specialist in Gynecology and Obstetrics
1, Physician, Specialist in Gynecology and Obstetrics
Nelson E. Arias-Ortiz ![]() 2, Physician, Doctor of Public Health
2, Physician, Doctor of Public Health
Walter A. Arboleda-Ruiz ![]() 3, Physician, Specialist in Gynecology and Obstetrics, Mastologist, Doctor in Design and Creation
3, Physician, Specialist in Gynecology and Obstetrics, Mastologist, Doctor in Design and Creation
1 Programa de Especialización en Ginecología y Obstetricia, Universidad de Caldas, Manizales, Colombia.
2 Grupo de Investigación en Promoción de la Salud y Prevención de la Enfermedad, Instituto de Investigaciones en Salud, Universidad de Caldas, Manizales, Colombia.
3 Grupo de investigación Materno-Perinatal de Caldas, Universidad de Caldas, SES-Hospital Universitario de Caldas, Manizales, Colombia.
ABSTRACT
Objective. To estimate the incidence, mortality and five-year survival of endometrial carcinoma in Manizales for the period 2003-2017.
Materials and methods. Observational, retrospective, population-based study, descriptive in scope. Incidence and mortality rates were adjusted by the direct method using the Segi world population as reference. Passive and active follow-up of the cases was carried out until completing 60 months or until the follow-up closing date. Survival was estimated using Kaplan-Meier functions and Cox models.
Results. 210 incident cases were observed in a population of 214.928 women. The average age at diagnosis was 61 years. The most frequent histological type was endometrioid, well differentiated. Most of the patients were affiliated to the contributory health insurance scheme and belonged to the middle socioeconomic level. The age-adjusted incidence rate was 5.7 new cases per 100,000 woman-years. Seventy-five deaths were identified, with greater mortality between 65-69 and 75-79 age groups. Overall survival was 95.1% at 12 months and 83.8% at 60 months. Statistically significant differences were found in survival in favor of epithelial histology, early stages at the time of diagnosis, and age at diagnosis less than 60 years.
Conclusions. Manizales follows the global pattern of rise in the age-adjusted incidence rate. Mortality is like that reported in other countries in the region. In Manizales, endometrial cancer survival was higher in patients with early diagnosis, less than 60 years of age, and with endometrioid histology.
Keywords: Colombia; Vital Statistics; Endometrioid adenocarcinoma; Endometrial neoplasms; Epidemiology; Incidence; Mortality; Survival, Populations records; Prevention and Control (source: MeSH NLM).
INTRODUCTION
According to Globocan (1), by 2020 more than 417,000 women were diagnosed with uterine cancer worldwide. Cancer of the uterine corpus is often referred to as endometrial cancer (EC) because more than 90% of cases originate in the endometrium (2). Prognostic factors for EC include age >60 years, histologic type, histologic grade, and staging at diagnosis (3,4).
In Colombia, incidence figures for EC differ according to the source. Estimates from the National Cancer Institute (INC), based on mortality data from the National Administrative Department of Statistics (DANE), report an age-adjusted incidence rate (AAIR) of 3.9 cases per 100,000 women-years (5). However, population-based cancer registries show higher figures with AAIR per 100,000 women-years ranging from 4.7 in Pasto (6) to 6.0 in Manizales (7) during the five-year period 2003-2007. Due to this discrepancy in incidence figures, it is necessary to update the reports with internationally comparable data.
The city of Manizales has the Manizales Population Cancer Registry (RPCa-M) which monitors the behavior of malignant neoplasms occurring in the resident population of the municipality and is indexed in the International Agency for Research on Cancer as a high-quality population-based registry with regional coverage (8). So far, a detailed analysis of the epidemiological behavior of EC has not been published, especially regarding survival from this cancer in Manizales. Descriptive studies such as this one allows us to understand the epidemiological behavior of the event and its risk factors in the local context, overcoming the limitations of traditional national estimates that hide the variability present within countries; likewise, having our own population-based data allows us to evaluate the performance of the healthcare system as a whole and to explore possible inequities as well as delay in access to healthcare according to the type of health insurance and socioeconomic level.
These data provide elements for adjusting specific programs within the framework of the Plan for Cancer Control in Colombia (9). The aim of our study was to estimate the incidence, mortality and 5-year survival rate of endometrial cancer in the population residing in Manizales during the period 2003- 2017.
|
KEY MESSAGES |
|
Motivation for the study: Data on endometrial cancer in Colombia are insufficient. Epidemiological indicators of this event in the population of Manizales are constructed as an input to analyze the performance of the health system and the strategies for the control of this type of cancer in the country. Main findings: In Manizales, incidence and mortality rates for endometrial cancer are low; eight out of ten patients survive to five years and survival is higher in women under 60 years of age, with early diagnosis and with tumors with epithelial histology. Implications: It is necessary to enssure timely diagnosis to improve survival. |
MATERIALS AND METHODS
Population
We conducted a descriptive, population-based, retrospective study.
The RPCa-M monitors the entire population residing in the urban and rural areas located inside the jurisdiction of the municipality of Manizales, estimated for 2018 at 434,403 inhabitants, of whom 229,296 are women and, of these, 124,499 are aged 35 years or older, according to the National Population and Housing Census (10). At the half of the analyzed period (year 2010), the female population in Manizales was 214,928 women according to the official DANE back projections. All incident cases recorded by the RPCa-M and deaths reported by DANE between January 1, 2003 and December 31, 2017 were included.
Procedures
Data on incident cases
Incident cases were obtained from the RPCa-M database using as a filter, the topographic code "C541" of the International Classification of Diseases for Oncology, 3rd edition, first revision. We included only cases of "endometrial cancer" and excluded tumors of the isthmus and uterine corpus not located in the endometrium. Staging was stablished for each patient based on the FIGO 2018 criteria (11). Information on sociodemographic, histologic, and clinical characteristics of the cases was collected from the RPCa-M database and medical records.
Data on deaths
We accessed the website of the official database of deaths published by DANE (12). The filters for department of residence (Caldas=017) and municipality of residence (Manizales=001) were applied to the national database, followed by the filter for the basic cause of death=C541.
Population data
Population data were obtained from the back projections (2003-2017) published by DANE (13) and disaggregated by calendar year, sex, and 18 five-year age groups (0 to 85 and older).
Survival estimates
The cases were followed up for a period of 60 months or until the closing date of follow-up (March 31, 2021) to identify the event of interest (death due to EC). The vital status of the patients was obtained by passive follow-up using the virtual health insurance platforms (Single Database of Affiliates -BDUA-, Administradora de los Recursos del Sistema General de Seguridad Social en Salud-ADRES-) and the National Registrar’s Office. Subsequently, the date and cause of death of the deceased were verified in the death certificates available in the Unified Registry of Affiliates - Births and Deaths (RUAF-ND) platform of the departmental health authority, which allowed us to have estimates of survival by specific cause. Survival analysis began with the 210 incident cases registered during the study period. We found 134 patients alive, 75 deceased and one patient lost to follow-up (0.5% of the total number of cases). Thirty-one patients were identified as having died from EC, 32 from another cause; for 11 deceased patients we did not obtain data on the cause of death. In the survival analysis, only deaths due to endometrial cancer were considered as events; the other cases were treated as censored.
Study variables
Age, histological type, type of health insurance, socioeconomic status and clinical stage were analyzed as predictors of survival (3). We established the cut-off point at 60 years for age based on other studies (2,4,14). The socioeconomic status of the dwelling was used as an indicator of social position. In Colombia, this indicator is defined in categories from one to six, according to the characteristics of the dwellings, where one and two correspond to the "low" socioeconomic level, three and four to "medium", and five and six to "high" (15).
The health insurance system in Colombia (which also applies to the municipality of Manizales) is funded by contributions from workers and employers (contributory regime). A small proportion (<5%) of the population working in certain public sectors has plans under the so-called "special or exceptional regime". The less favored population is covered by a subsidized system, supported through taxes (16). The RPCa-M records information on patients from all insurance plans and even the population not covered by health insurance; the data for this variable were verified case by case in the public databases of the Colombian health system.
Statistical analysis
Analyses were carried out using Microsoft Excel and Stata 14 (Stata Corporation, College Station, Texas, USA). Central and dispersion measures were used for numerical variables, and relative frequencies for categorical variables. During the bivariate analysis, we used the chi-square test to compare the distribution of clinical stage according to the type of health insurance and socioeconomic status. Age-adjusted incidence and mortality rates were calculated for the Segi world population (standard world population proposed by Segi in 1954, adjusted by Doll in 1966 and which has been used in international comparative studies of cancer epidemiology) using the direct method. Survival estimates were obtained by the Kaplan Meier method and comparisons between categories of variables were established using the Logrank test. Multivariate analysis was carried out using Cox proportional hazards models, but the results of these models are presented as supplementary material since the number of observations (both cases and deaths from the event) was very low and did not allow us to obtain precise estimates of the independent effect of the variables.
Ethical Aspects
This study complied with the parameters stablished by the Declaration of Helsinki of the World Medical Association and Resolution 8430 of 1993 of the Colombian Ministry of Health. This study was considered to have minimal risk since there was no biological manipulation of the variables and did not include procedures that would threaten the physical and moral integrity of the subjects. It was approved by the Ethics Committee of the Faculty of Health Sciences (Act 004 of 2020 consecutive CBCS-015).
RESULTS
Table 1. shows the distribution of incident cases and deaths according to the study variables.
Table 1. Distribution of incident cases and deaths due to endometrial cancer. Manizales, 2003-2017.
|
Variable |
Incident cases |
Cases |
|||
|
n |
% |
n |
% |
||
|
Total |
210 |
100.0 |
75 |
100,0 |
|
|
Age at diagnostic |
|
|
|
|
|
|
<60 years |
89 |
42.4 |
22 |
29.3 |
|
|
60 or older |
121 |
57.6 |
53 |
707 |
|
|
Histology |
|
|
|
|
|
|
Adenocarcinoma |
202 |
96.2 |
ND |
||
|
Other a |
8 |
3.8 |
ND |
||
|
Clinical stage |
|
|
|
|
|
|
I |
73 |
34.8 |
ND |
||
|
II |
23 |
11.0 |
ND |
||
|
III |
29 |
13.8 |
ND |
||
|
IV |
31 |
14.8 |
ND |
||
|
No data |
54 |
25.6 |
ND |
||
|
Health insurance |
|
|
|
||
|
Contributive |
160 |
76.2 |
52 |
69.3 |
|
|
Subsided |
40 |
19.0 |
17 |
22.7 |
|
|
Special/exception/prepaid |
5 |
2.4 |
6 |
8.0 |
|
|
Not affiliated |
2 |
1.0 |
0 |
0.0 |
|
|
No data |
3 |
1.4 |
0 |
0.0 |
|
|
Socioeconomic status |
|
|
|
||
|
Low |
37 |
17.6 |
ND |
||
|
Medium |
117 |
55.7 |
ND |
||
|
High |
20 |
9.5 |
ND |
||
|
No data |
36 |
17.2 |
ND |
||
a Includes endometrial stromal tumors, mixed tumors and unspecified tumors according to the WHO histological classification 2014.
ND: No data available for the variable in the database of deaths of the National Administrative Department of Statistics (DANE).
Deaths do not necessarily correspond to patients included as incident cases in the study period. Some deaths may correspond to incident patients outside the study time window, or patients residing outside the municipality of Manizales at the time of diagnosis who are not included as incident cases from the population of Manizales.
Incidence
The mean age at diagnosis was 61.2 years with a standard deviation of 10.1 years, minimum age of 30 and maximum age of 85 years. The most valid criterion for diagnosis was the anatomopathological study in 100% of the cases. Epithelial tissue, endometrioid subtype was the predominant histological type (Supplementary Table 2). The most frequent histologic stage was well differentiated (stage 1) in 44.8% of the patients.
Table 2. Estimates of cause-specific survival to endometrial cancer according to variables of interest. Manizales 2003-2017.
|
|
Cases (N) |
Deaths (n) |
12 m |
24 m |
36 m |
48 m |
60 m |
Logrank test |
|
All cases |
210 |
31 |
95.1 |
88.3 |
86.1 |
84.4 |
83.8 |
|
|
Time of diagnostic (5-year period) |
|
|
|
|
|
|
|
|
|
2003-2007 |
62 |
4 |
100.0 |
94.2 |
94.2 |
94.2 |
94.2 |
|
|
2008-2012 |
67 |
11 |
97.0 |
90.3 |
87.0 |
85.2 |
83.5 |
p=0.110 |
|
2013-2017 |
81 |
16 |
90.1 |
83.9 |
82.6 |
79.8 |
79.8 |
|
|
Health insurance a |
|
|
|
|
|
|
|
|
|
Contributive |
160 |
23 |
94.9 |
89.6 |
88.2 |
86.7 |
86.0 |
|
|
Subsided |
40 |
6 |
97.4 |
88.4 |
85.0 |
81.3 |
81.3 |
p=0.960 |
|
Special/exception/prepaid |
5 |
1 |
100.0 |
80.0 |
80.0 |
80.0 |
80.0 |
|
|
Not affiliated |
2 |
0 |
100.0 |
100.0 |
100.0 |
100.0 |
100.0 |
|
|
Socioeconomic status b |
|
|
|
|
|
|
|
|
|
Low |
37 |
6 |
97.1 |
85.4 |
85.4 |
81.7 |
81.7 |
|
|
Medium |
117 |
18 |
95.6 |
89.0 |
85.9 |
84.9 |
83.7 |
p=0.990 |
|
High |
20 |
3 |
94.7 |
94.7 |
94.7 |
88.8 |
88.8 |
|
|
Age at diagnostic |
|
|
|
|
|
|
|
|
|
<60 years |
89 |
8 |
97.8 |
94.3 |
93.1 |
91.9 |
91.9 |
|
|
60 or older |
121 |
23 |
93.0 |
84.5 |
82.4 |
80.2 |
79.0 |
p=0.016 |
|
Histology |
|
|
|
|
|
|
|
|
|
Adenocarcinoma |
202 |
27 |
96.4 |
90.5 |
88.8 |
86.9 |
86.3 |
|
|
Other and not specified c |
8 |
4 |
62.5 |
46.9 |
46.9 |
46.9 |
46.9 |
|
|
Clinical stage d |
|
|
|
|
|
|
|
|
|
I |
73 |
2 |
98.6 |
97.2 |
97.2 |
97.2 |
97.2 |
|
|
II |
23 |
4 |
100.0 |
91.3 |
87.0 |
81.8 |
81.8 |
p <0.001 |
|
III |
29 |
7 |
96.6 |
85.5 |
81.6 |
77.6 |
77.6 |
|
|
IV |
31 |
11 |
82.7 |
69.0 |
60.4 |
518 |
51.8 |
|
a Three cases without data are excluded; b 36 cases without data are excluded; c includes endometrial stromal tumors, mixed tumors, and unspecified tumors according to the World Health Organization 2014 histological classification; d 54 cases without data were excluded.
Statistically significant differences were found in clinical staging according to the health insurance type (p = 0.011), but not according to socioeconomic status (p = 0.881). Figure 1 summarizes the AAIR by EC according to period of diagnosis. No statistically significant differences in incidence were observed in the three five-year periods studied.
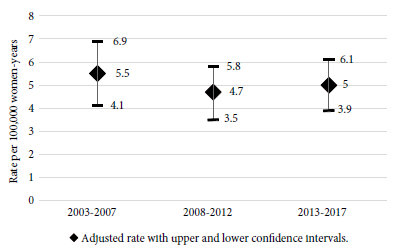
Figure 1. Age-adjusted endometrial cancer incidence rate by time of diagnosis (5-year period). Manizales 2003-2017.
Mortality
Nearly 50% of deaths occurred in women between 55 and 69 years of age. In the period between 2013 to 2017 the highest risk of dying from EC was found in women between 70 and 84 years, while in the previous five-year periods, mortality was mostly observed in women between 65 and 74 years. Figure 2 shows the AAIR according to the period of diagnosis; there is an apparent increasing trend in mortality in the last five-year period, but it’s not statistically significant.
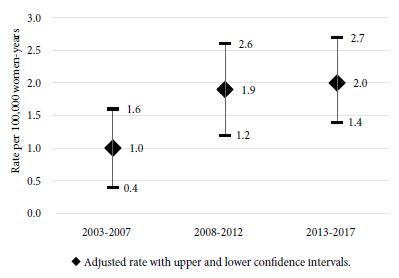
Figure 2. Age-adjusted endometrial cancer mortality rate by occurrence (5-year period). Manizales, 2003-2017.
Survival
EC-specific survival was 83.8% at 60 months of follow-up. Figure 3 shows the Kaplan-Meier survival plot for the entire set of cases analyzed. Table 2 summarizes the survival estimates according to the variables of interest. Five-year survival in patients diagnosed at stage I was almost double of that observed in for stage IV patients. Similar differences were obtained for survival by histologic type in those patients with epithelial tumors compared to other histologic types. The difference in survival was 12 percentage points in women younger than 60 years. The simultaneous effects of the predictors of survival are presented in Supplementary Table 1.
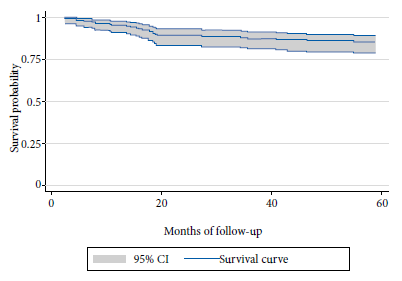
Figure 3. Kaplan-Meier plot for endometrial cancer survival (all cases) Manizales, 2003-2017.
DISCUSSION
This research is the first detailed description of incidence, mortality and survival due to EC in Manizales. Age at diagnosis and distribution by histological type are similar to those reported in other studies (4,5,17). The distribution of incident cases according to health insurance type and socioeconomic status is consistent with the behavior of these variables in the general population of Manizales.
In Manizales, the frequency of early stages is low (61.5 vs. 77.2%) when compared with hospital case series (5,18). The percentage of missing data for this variable is significant, which may be a reflection of the barriers to patient access to laboratory tests for the disease, as well as an indicator of the lack of the information in the clinical records, particularly for cases diagnosed during the first five years.
Regarding incidence, Manizales has a low risk of developing the disease, which is similar to other cities in Colombia and the world, (6,19-22). In regards to mortality, AAIR per 100,000 women-years doubled in a decade, from 1.0 death in the period 2003 - 2007 to 2.0 deaths in 2013 - 2017; although this variation did not reach statistical significance, it is similar to the increase reported in other studies (4,23).
The five-year specific survival rate obtained in Manizales (83.8%) is similar to the relative survival for uterine corpus cancer (81%) reported in 2019 by the American Cancer Society as well as the one reported by the United States Surveillance, Epidemiology and End Results (SEER) Program (83%) for white women (2), which is plausible considering that a large part of the population of Manizales is white or mestizo.
In Manizales, age was a significant predictor of survival in the unadjusted analysis and is consistent with the literature (4,14), although the significance was not sustained during the multivariate analysis. Regarding stage at diagnosis, the distribution of survival is very similar to that reported by SEER, with lower survival in advanced stages (2).
In our study, tumor histology was not a predictor of survival independent of age and clinical stage at diagnosis, which differs from the concept that survival is lower when EC histology is not epithelial (4,5,14,18,23). Recent research shows that the risk profile of this type of cancer is constructed from the molecular characteristics of the tumor (24-26), which classifies tumors according to the presence of mutations, instability in microsatellites and expression of estrogen and progestin receptors, and HER2 (human epidermal receptor 2); these characteristics define the differences in the clinical behavior of the disease. Therefore, it is important for cancer registries to collect these new variables in order to adequately analyze EC survival.
Unlike what has been observed in other cancers such as cervical and breast cancer, socioeconomic status and health insurance type did not show a significant effect on survival.
One of the limitations of the study is that although we used the designation "population-based study", it is not plausible to assume perfect completeness (100%) in the capture of new cases, so the real incidence in the population may be underestimated. Nevertheless, the RPCa-M meets the quality standards required for the publication of data in the "Cancer Incidence in Five Continents" and previous quality assessments qualify the RPCa-M as a high-quality registry (27). Undoubtedly, the main limitation of the analyses is the low number of observations in some categories of the studied variables, which should lead to a cautious interpretation of the results, particularly the survival estimates obtained using the Cox proportional hazards model, as they are not very precise. In addition, a significant percentage of missing data was found for clinical staging and socioeconomic status, as well as for the specific cause of death.
Our results contribute to the knowledge of the behavior of endometrial cancer in the Colombian and Latin American context. The data we obtained are useful for the country because they allow identifying possibilities for adjustments in medical care aimed at improving timely diagnosis based on adequate diagnostic suspicion, which can reduce premature deaths among women in Manizales. Eight out of ten women survived at five years, which shows that the Colombian health system effectively diagnoses and treats these patients. However, our results may differ from what occurs in other Colombian populations with less health infrastructure, so it is necessary to conduct studies in other cities with adequate population registries to consolidate knowledge about the capacity of the health system to provide adequate care to patients with EC.
In conclusion, the risk of becoming ill and dying from endometrial cancer in Manizales is low and similar to what has been reported for other populations in Colombia and the world. Five-year survival rates show that the prognosis is good overall, but there is still room for interventions aimed at increasing the proportion of cases diagnosed in early stages, since this is the most important prognostic variable. It is necessary to continue improving the quality of the data collected by the RPCa-M.
Authors’ contributions: The three authors participated in the conception and design of the research. MCMG and NEAO carried out the data collection and analysis. MCMG drafted the first version of the manuscript. All authors reviewed and approved the final version of the article.
Conflicts of interest: The authors declare that they have no conflicts of interest.
Funding: The research was co-funded by the Universidad de Caldas and the Instituto Nacional de Cancerología de Colombia.
Supplementary material: Available in the electronic version of the RPMESP.
REFERENCIAS BIBLIOGRÁFICAS
1. IARC. Globocan. Cancer today [Internet]. Global cancer observatory. Maps view. 2020 [citado el 28 de junio de 2021]. Disponible en: https://gco.iarc.fr.
2. Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69(5):363–85. doi: 10.3322/caac.21565.
3. Cormier B, Rozenholc AT, Gotlieb W, Plante M, Giede C. Sentinel lymph node procedure in endometrial cancer: A systematic review and proposal for standardization of future research. Gynecol Oncol. 2015;138(2):478–85. doi: 10.1016/j.ygyno.2015.05.039.
4. Koh WJ, Abu-Rustum NR, Bean S, Bradley K, Campos SM, Cho KR, et al. Uterine Neoplasms, Version 1. 2018, NCCN Clinical Practice Guidelines in Oncology. NCCN Clin Pract Guidel Oncol. 2018;16(2):170–9. doi: 10.6004/JNCCN.2018.0006.
5. Ruiz J. Características clínicas e histopatológicas de pacientes con carcinoma epitelial de endometrio tratadas con cirugía en el instituto nacional de cancerología (INC) durante agosto-2007 a agosto 2012. Universidad Militar Nueva Granada; 2012.
6. Yépez MC, Bravo LM, Bravo LE, Hidalgo-Troya A, Jurado DM. Cancer incidence and mortality in the municipality of Pasto, 1998 - 2007. Colomb Méd. 2012;43(4):256–66. doi: 10.25100/cm.v43i4.1179.
7. López Guarnizo G, Arias Ortiz N, Arboleda Ruiz W. Cancer incidence and mortality in Manizales 2003-2007. Colomb Méd. 2012;43(4):281–9. doi: 10.25100/cm.v43i4.1197.
8. Piñeros M, Abriata MG, Mery L, Bray F. Cancer registration for cancer control in Latin America: a status and progress report. Rev Panam Salud Publica. 2017;41(5):e2. doi: 10.26633/RPSP.2017.2.
9. Ministerio de Salud y Protección Social de Colombia, Instituto Nacional de Cancerología . Plan Decenal para el Control del Cáncer en Colombia, 2012-2021. Bogotá, D.C.; 2012. 1–124 p.
10. Departamento Administrativo Nacional de Estadísticas. Censo Nacional de Población y Vivienda. Población ajustada por cobertura. 2018.
11. Amant F, Raza M, Koskas M, Creutzberg C. FIGO cancer report 2018. Cancer of the corpus uteri. Int J Gynecol Obstet. 2018;142(S2):37–50. doi: 10.1002/ijgo.12612.
12. Departamento Administrativo Nacional de Estadísticas. Microdatos anonimizados de estadísticas vitales [Internet]. Colecciones. Estadísticas Vitales. 2021 [citado el 5 de marzo de 2021]. Disponible en: http://microdatos.dane.gov.co/index.php/catalog/MICRODATOS/about_collection/22/5.
13. Departamento Administrativo Nacional de Estadísticas. Proyecciones de población [Internet]. Estadísticas por tema. Demografía y población. 2020 [citado el 11 de noviembre de 2020]. Disponible en: https://www.dane.gov.co/index.php/estadisticas-por-tema/demografia-y-poblacion/proyecciones-de-poblacion.
14. Boggess J, Kilgore J. Uterine Cancer. En: Abeloff’s Clinical Oncology. 5a ed. 2014. p. 1575–91.
15. Arias Ortiz NE, De Vries E. Health inequities in cancer survival in Manizales , Colombia: a population-based study. Colomb Med [Internet]. 2018 [citado el 15 de febrero de 2019];49(1):63–72. doi: 10.25100/cm.v49i1.3629.
16. Ministerio de Salud y Protección Social. Cartilla Aseguramiento al Sistema General de Seguridad Social en Salud. Bogotá, Colombia: Imprenta Nacional de Colombia; 2014. 1–63 p.
17. Lloyd R, Osamura R, Günter K, Juan R. World Health Organization Classification of Tumours, 4th Edition. 2017. 46–47 p.
18. Fernández-Mercado RS, Miranda-Mejía MA, Fletcher-Prieto AV, Rodríguez-Gallego JA, Mora-Padilla E, Orostegui-Correa S, et al. Prevalencia del compromiso ganglionar en pacientes con cáncer de endometrio, Colombia 2009-2016: análisis exploratorio de factores asociados. Rev Colomb Obstet Ginecol. 2020;71(2):38–44. doi: 10.18597/rcog.3450.
19. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. [Internet]. CA CANCER J CLIN. 2018 [citado el 13 de abril de 2020]. p. 394–424. doi: 10.3322/caac.21492.
20. IARC. Incidence, Mortality and Prevalence by cancer site, Colombia. Global cancer observatory. 2018.
21. Uribe C, Osma S, Herrera V. Cancer incidence and mortality in the Bucaramanga metropolitan area, 2003-2007. Colomb Méd. 2012;43(4):290–7. doi: 10.25100/cm.v43i4.1196.
22. Pérez CJU, Gómez SES, Sánchez CMH. Cancer incidence and mortality in Bucaramanga, Colombia. 2008-2012. Colomb Med. 2018;49(1):73–80. doi: 10.25100/cm.v49i1.3632.
23. National Cancer Institue. Uterine Cancer — Cancer Stat Facts [Internet]. Cancer Statistics Facts. 2020. Disponible en: https://seer.cancer.gov/statfacts/html/corp.html#skipnav.
24. Wang C, Tran DA, Fu MZ, Chen W, Fu SW, Li X. Estrogen receptor, progesterone receptor, and HER2 receptor markers in endometrial cancer. J Cancer. 2020;11(7):1693–701. doi: 10.7150/jca.41943.
25. Franco G, Odetto D, Bianchi F, Rossini M, Di Fiore H, Navarini R, et al. Consenso de ginecología FASGO 2019. "Cáncer de endometrio." Com Consensos Fed Argentina Soc Ginecol y Obstet FASGO. 2019.
26. Chang Z, Talukdar S, Mullany SA, Winterhoff B. Molecular characterization of endometrial cancer and therapeutic implications. Curr Opin Obstet Gynecol. 2019;31(1):24–30. doi: 10.1097/GCO.0000000000000508.
27. Arias-Ortiz N, López-Guarnizo G. Evaluación de Calidad de los Datos del Registro Poblacional de Cáncer de Manizales, Colombia. Rev Colomb Cancerol. 2013 [citado el 12 de abril de 2020];17(4):132–41. doi: 10.1016/S0123-9015(13)70160-4.
Correspondence: Nelson Enrique Arias Ortiz; nelson.arias@ucaldas.edu.co
Cite as: Montoya-González MC, Arias-Ortiz NE, Arboleda-Ruiz W. Incidence, mortality and survival of endometrial cancer in Manizales, Colombia 2003-2017. Rev Peru Med Exp Salud Publica. 2021;38(4):562-8. doi: https://doi.org/10.17843/rpmesp.2021.384.8892.
Received: 09/07/2021
Approved: 24/11/2021
Online: 22/12/2021