Evaluación del neurodesarrollo en niños con exposición intrauterina al virus del Zika: estudio observacional transversal
DOI:
https://doi.org/10.17843/rpmesp.2023.403.12880Palabras clave:
Infección por el virus del Zika, Evaluación del Desarrollo, Estudio Observacional, Desarrollo Infantil, Pruebas NeuropsicológicasResumen
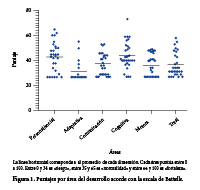
El virus del Zika produce desenlaces adversos para el desarrollo del sistema nervioso. Este estudio describe el neurodesarrollo cognitivo, adaptativo, comunicativo, social y motor de niños expuestos intrauterinamente al virus del Zika y hace una evaluación del neurodesarrollo con la escala de Battelle a los tres años después del nacimiento. Participaron 30 niños con una media de edad al momento de la evaluación de 37,5 (RIC: 35,7–39,2) meses. Se halló una edad equivalente en meses en las áreas: motora 25,8 (DE:
7,8), adaptativa 26,7 (DE: 5,8), comunicativa 30,2 (DE: 6,9), personal social 33,5 (DE: 8,3) y cognitiva 35,6 (DE: 5,9). Los niños presentaron retraso en el desarrollo para la edad cronológica, 25 niños presentaban retraso en una de las cinco áreas evaluadas. Una alta proporción de niños expuestos al virus del Zika durante la gestación presentaron retraso en el desarrollo, principalmente en el dominio adaptativo y motor.
Descargas
Referencias
Cucunuba ZM. De la epidemia de Zika en Latinoamérica y la toma de decisiones bajo incertidumbre. Salud UIS. 2016;48 (2):158–60.
Méndez N, Oviedo-Pastrana M, Mattar S, Caicedo-Castro I, Arrieta G. Zika virus disease, microcephaly and Guillain-Barré syndrome in
Colombia: epidemiological situation during 21 months of the Zika virus outbreak, 2015-2017. Arch Public Health. 2017;75:65. doi: 10.1186/s13690-017-0233-5.
Moore CA, Staples JE, Dobyns WB, Pessoa A, Ventura CV, Fonseca EB da, et al. Characterizing the pattern of anomalies in congenital Zika syndrome for pediatric clinicians. JAMA Pediatr. 2017;171(3):288. doi: 10.1001/jamapediatrics.2016.3982.
Haby MM, Pinart M, Elias V, Reveiz L. Prevalence of asymptomatic Zika virus infection: a systematic review. Bull World Health Organ.
;96(6):402-413D. doi: 10.2471/BLT.17.201541.
Marbán-Castro E, Vazquez Guillamet LJ, Pantoja PE, Casellas A, Maxwell L, Mulkey SB, et al. Neurodevelopment in normocephalic
children exposed to Zika virus in utero with no observable defects at birth: A systematic review with meta-analysis. Int J Environ Res Public Health. 2022;19(12):7319. doi: 10.3390/ijerph19127319.
Faiçal AV, de Oliveira JC, Oliveira JVV, de Almeida BL, Agra IA, Alcantara LCJ, Acosta AX, de Siqueira IC. Neurodevelopmental delay in normocephalic children with in utero exposure to Zika virus. BMJ Paediatr Open. 2019;3(1). doi: 10.1136/bmjpo-2019-000486.
Lebov JF, Brown LM, MacDonald PDM, Robertson K, Bowman NM, Hooper SR, et al. Review: Evidence of neurological sequelae in children with acquired Zika virus infection. Pediatr Neurol. 2018;85:16–20. doi: 10.1016/j.pediatrneurol.2018.03.001.
Saad T, PennaeCosta AA, de Góes FV, de Freitas M, de Almeida JV, de Santa Ignêz LJ, et al. Neurological manifestations of congenital Zika virus infection. Childs Nerv Syst. 2018;34(1):73–8. doi: 10.1007/s00381-017-3634-4.
Marbán-Castro E, Enguita-Fernàndez C, Romero-Acosta KC, Arrieta GJ, Marín-Cos A, Mattar S, et al. “One feels anger to know there is no one to help us!”. Perceptions of mothers of children with Zika virus-associated microcephaly in Caribbean Colombia: A qualitative study. PLoS Negl Trop Dis. 2022;16(4):e0010328. doi: journal.pntd.0010328.
Hcini N, Kugbe Y, Rafalimanana ZHL, Lambert V, Mathieu M, Carles G, et al. Association between confirmed congenital Zika infection at birth and outcomes up to 3 years of life. Nat Commun. 2021;12(1). doi: 10.1038/s41467-021-23468-3.
Aguilar Ticona JP, Nery N, Ladines-Lim JB, Gambrah C, Sacramento G, de Paula Freitas B, et al. Developmental outcomes in children exposed to Zika virus in utero from a Brazilian urban slum cohort study. PLoS Negl Trop Dis. 2021;15(2):e0009162. doi: 10.1371/journal.pntd.0009162.
Stringer EM, Martinez E, Blette B, Toval Ruiz CE, Boivin M, Zepeda O, et al. Neurodevelopmental outcomes of children following in utero exposure to Zika in Nicaragua. Clin Infect Dis. 2021;72(5):e146–53. doi: 10.1093/cid/ciaa1833.
Cunha ACB, Berkovits MD, Albuquerque KA. Developmental assessment with young children: A systematic review of Battelle
studies. Infants Young Child. 2018;31(1):69–90. doi: 10.1097/IYC.0000000000000106.
Duttine A, Smythe T, Calheiro de Sá MR, Ferrite S, Moreira ME, Kuper H. Development and assessment of the feasibility of a Zika
family support programme: a study protocol. Wellcome Open Res. 2019;4:80. doi: 10.12688/wellcomeopenres.15085.1.
Valdes V, Zorrilla CD, Gabard-Durnam L, Muler-Mendez N, Rahman ZI, Rivera D, et al. Cognitive development of infants exposed to the Zika virus in Puerto Rico. JAMA Netw Open. 2019;2(10):e1914061. doi: 10.1097/iyc.0000000000000106.
Clark GF, Kingsley KL. Occupational therapy practice guidelines for early childhood: Birth-5 years. Am J Occup Ther.
;74(3):7403397010p1–42. doi: 10.5014/ajot.2020.743001.
Rubio-Codina M, Araujo MC, Attanasio O, Muñoz P, Grantham-McGregor S. Concurrent Validity and Feasibility of Short
Tests Currently Used to Measure Early Childhood Development in Large Scale Studies. PLoS One. 2016;11(8):e0160962. doi:10.1371/journal.pone.0160962.
Aguilar Ticona JP, Nery N, Doss-Gollin S, Gambrah C, Lessa M, Rastely-Júnior V, et al. Heterogeneous development of children with
Congenital Zika Syndrome-associated microcephaly. PLoS One. 2021;16(9):e0256444. doi: 10.1371/journal.pone.0256444.
De los Reyes-Aragon CJ, Amar Amar J, De Castro Correa A, Lewis Harb S, Madariaga C, Abello-Llanos R. The care and development of children living in contexts of poverty. J Child Fam Stud. 2016;25(12):3637–43. doi: 10.1007/s10826-016-0514-6.
Grant R, Fléchelles O, Tressières B, Dialo M, Elenga N, Mediamolle N, et al. In utero Zika virus exposure and neurodevelopment at 24 months in toddlers normocephalic at birth: a cohort study. BMC Med. 2021;19(1). doi: 10.1186/s12916-020-01888-0.
Esper NB, Franco AR, Soder RB, Bomfim RC, Nunes ML, Radaelli G, et al. Zika virus congenital microcephaly severity classification
and the association of severity with neuropsychomotor development. Pediatr Radiol. 2022;52(5):941–50. doi: 10.1007/s00247-022-05284-z.
Martins MM, Alves da Cunha AJL, Robaina JR, Raymundo CE, Barbosa AP, Medronho R de A. F et al, neonatal, and infant outcomes
associated with maternal Zika virus infection during pregnancy: A systematic review and meta-analysis. PLoS One. 2021;16(2):e0246643.
doi: 10.1371/journal.pone.0246643.
Alves LV, Paredes CE, Silva GC, Mello JG, Alves JG. Neurodevelopment of 24 children born in Brazil with congenital Zika syndrome in
: a case series study. BMJ Open. 2018;8(7):e021304. doi: 10.1136/bmjopen-2017-021304.
Operto FF, Viggiano A, Perfetto A, Citro G, Olivieri M, Simone V de, et al. Digital devices use and fine motor skills in children between 3–6 years. Children (Basel). 2023;10(6):960. doi: http://dx.doi.org/10.3390/children10060960.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2023 Victor H. Estupiñan-Perez; Angela M. Jiménez-Urrego, Freiser E. Cruz-Mosquera, Alejandro Botero-Carvajal

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.