Factores asociados al uso de psicofármacos por estudiantes de una universidad pública brasileña
DOI:
https://doi.org/10.17843/rpmesp.2024.414.13858Palabras clave:
Utilización de Medicamentos, Psicotrópicos, Salud del Estudiante, Universidad, BrasilResumen
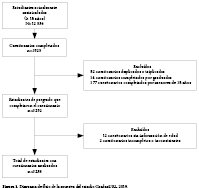
Objetivo. Analizar el consumo de medicamentos psicotrópicos y sus factores asociados en estudiantes universitarios, estratificado segun sexo. Materiales y Métodos. Se realizó un estudio transversal con estudiantes de pregrado de una universidad pública de Brasil. El instrumento fue un cuestionario autoadministrado en línea. La variable de resultado fue el uso de medicamentos psicotrópicos, con base en el sistema de clasificación Anatómico Terapéutico Químico (ATC) y las variables de exposición fueron socidemográficas, académicas y relacionadas con la salud. La asociación entre las variables de exposición y el resultado se verificaron mediante el cálculo de razones de prevalencia y sus intervalos de confianza al 95%. Resultados. El 12,2% (n=396) de los 3238 participantes refirieron consumir psicofármacos, la mayoría fueron mujeres (78,3%). La prevalencia de consumo de psicotrópicos fue mayor entre los estudiantes con acceso a seguro de salud, diagnóstico de depresión y diagnóstico de ansiedad. También fue mayor en el grupo de mujeres que informaron consumir drogas ilícitas en los últimos tres meses y en el grupo de hombres que informaron estar insatisfechos o muy insatisfechos con su rendimiento académico. Se detectó una menor frecuencia de uso de psicofármacos entre las mujeres que consumen alcohol semanalmente. Conclusiones. Los resultados indican una mayor frecuencia de consumo de medicamentos psicotrópicos en las mujeres, así como en los estudiantes con acceso
al seguro de salud, diagnóstico de depresión y diagnóstico de ansiedad, independientemente del sexo.
Descargas
Referencias
Nogueira MJ, Seabra P, Alves P, Teixeira D, Carvalho JC, Sequeira C. Predictors of positive mental health in higher education students.
A cross-sectional predictive study. Perspect Psychiatr Care. 2022;58(4):2942–9. doi: 10.1111/ppc.13145.
Castaldelli-Maia JM, Lewis T, Marques dos Santos N, Picon F, Kadhum M, Farrell SM, et al. Stressors, psychological distress, and mental health problems amongst Brazilian medical students. Int Rev Psychiatry. 2019;31(7–8):603–7. doi: 10.1080/09540261.2019.1669335.
Sheldon E, Simmonds-Buckley M, Bone C, Mascarenhas T, Chan N, Wincott M, et al. Prevalence and risk factors for mental health
problems in university undergraduate students: A systematic review with meta-analysis. J Affect Disord. 2021;287:282–92. doi:
1016/j.jad.2021.03.054.
Beroíza-Valenzuela F. The challenges of mental health in Chilean university students. Front Public Heal. 2024;12:1297402. doi:
3389/fpubh.2024.1297402.
Lima AMS, Leal R, Fernandes dos Santos V, Leal L, Rocha A, Silva E, et al. Prevalência da Depressão nos Acadêmicos da Área de Saúde. Psicol Ciênc Prof. 2019;39:e187530. doi: 10.1590/1982-3703003187530.
Pacheco JPG, Giacomin HT, Tam WW, Ribeiro TB, Arab C, Bezerra IM, et al. Mental health problems among medical students in
Brazil: a systematic review and meta-analysis. Rev Bras Psiquiatr. 2017;39(4):369–78. doi: 10.1590/1516-4446-2017-2223.
Bojanić I, Sund ER, Bjerkeset O, Sivertsen B, Sletvold H. Psychological Distress and Use of Psychotropic Drugs Among University
Students—the SHoT Study, Norway. Front Psychiatry. 2021;12717955. doi: 10.3389/fpsyt.2021.717955.
Fond G, Bourbon A, Boucekine M, Messiaen M, Barrow V, Auquier P, et al. First-year French medical students consume antidepressants and anxiolytics while second-years consume non-medical drugs. J Affect Disord. 2020;265:71–6. doi: 10.1016/j.jad.2020.01.035.
Sobral de Luna I, Augusta Grigoli Dominato A, Ferrari F, Lobo da Costa A, Christhinie Pires A, da Silva Ximendes G. Consumo de psicofármacos entre alunos de medicina do primeiro e sexto ano de uma universidade do estado de São Paulo. Colloq Vitae. 2018;10(1):22–8. doi: 10.5747/cv.2018.v10.n1.v216.
Fasanella NA, Custódio CG, Cabo JS, Andrade GS, Almeida FA, Pavan MV. Use of prescribed psychotropic drugs among medical students and associated factors: a cross-sectional study. Sao Paulo Med J. 2022;140(5):697–704. doi: 10.1590/1516-3180.2021.0566.R2.05012022.
Scheifes A, Walraven S, Stolker JJ, Nijman HLI, Egberts TCG, Heerdink ER. Adverse events and the relation with quality of life in adults with intellectual disability and challenging behaviour using psychotropic drugs. Res Dev Disabil. 2016;49–50:13–21. doi: 10.1016/j.ridd.2015.11.017.
SenthilKumar G, Mathieu NM, Freed JK, Sigmund CD, Gutterman DD. Addressing the decline in graduate students’ mental well-being.
Am J Physiol - Hear Circ Physiol. 2023;325(4):H882–7. doi: 10.1152/ajpheart.00466.2023.
Bacigalupe A, Martín U. Gender inequalities in depression/anxiety and the consumption of psychotropic drugs: are we medicalising
women’s mental health? Scand J Public Health. 2021;49(3):317–24. doi: 10.1177/1403494820944736.
Quintana MI, Andreoli SB, Peluffo MP, Ribeiro WS, Feijo MM, Bressan RA, et al. Psychotropic drug use in São Paulo, Brazil: an epidemiological survey. PLoS One. 2015; 10(8):e0135059. doi: 10.1371/journal.pone.0135059.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al. Strengthening the reporting of observational
studies in epidemiology (StroBE) statement: guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–7. doi:
7326/0003-4819-147-8-200710160-00010.
Frazon AG. Síndrome de burnout e o consumo de álcool e de substâncias ilícitas por estudantes universitários [Tese]. Londrina: Universidade Estadual de Londrina; 2021. 184 p.
World Health Organization. ATC/DDD Index 2022. Geneva: OMS; 2022. [cited 2023 Sept 21]. Available from: https://www.whocc.no/atc_ddd_index/.
Liu Y, Zhang N, Bao G, Huang Y, Ji B, Wu Y, et al. Predictors of depressive symptoms in college students: A systematic review and
meta-analysis of cohort studies. J Affect Disord. 2019;244:196–208. doi: 10.1016/j.jad.2018.10.084.
Bacigalupe A, Martín U. Gender inequalities in depression/anxiety and the consumption of psychotropic drugs: Are we medicalising
women’s mental health? Scand J Public Health. 2021;49(3):317-324. doi: 10.1177/1403494820944736.
Santos LH, Silveira MM. Uso de psicofármacos por estudantes de psicologia. Cad Bras Saúde Mental. 2019;11(29):1–12. doi: 10.5007/cbsm.v11i29.69801.
Câmara H, Rocha C, Balteiro J. Grau de conhecimento e consumo de psicofármacos dos alunos da Escola Superior de Tecnologia da
Saúde de Coimbra. Rev Port Saude Publica. 2011;29(2):173–9. doi: 10.1016/S0870-9025(11)70021-9.
Berchtold A, Genre N, Panese F. Uses of psychotropic drugs by university students in Switzerland. PLoS One. 2024;19(6):e0305392. doi: 10.1371/journal.pone.0305392
Marchi KC, Bárbaro AM, Miasso AI, Tirapelli CR. Ansiedade e consumo de ansiolíticos entre estudantes de enfermagem de uma universidade pública. Rev Eletr Enf. 2013;15(3):731–9. doi: 10.5216/ree.v15i3.18924.
Istilli PT, Miasso AI, Padovan CM, Crippa JA, Tirapelli CR. Antidepressants: knowledge and use among nursing students. Rev Lat-Am
Enfermagem. 2010;18(3):421–8. doi: 10.1590/S0104-11692010000300018.
Souza GCRM, Vasques JS, Rodrigues LAC, Komatsu AV, Silva JL, Maniglia FP. Uso de ansiolíticos e antidepressivos entre estudantes
de medicina de uma universidade. Psico. 2022;53(1):e38105. doi: 10.15448/1980-8623.2022.1.38105.
Bielli A, Bacci P, Bruno G, Calisto N. Cambiar para que todo siga igual: mujeres y psicofármacos en Uruguay. Rev Estud Fem. 2023;31(1): e93197. doi: 10.1590/1806-9584-2023v31n193197.
Lun KWC, Chan CK, Ip PKY, Ma SYK, Tsai WW, Wong CS, et al. Depression and anxiety among university students in Hong Kong. Hong Kong Med J. 2018;24(5):466–72. doi: 10.12809/hkmj176915.
Parker G, Brotchie H. Gender differences in depression. Int Rev Psychiatry. 2010;22(5):429–36. doi: 10.3109/09540261.2010.492391.
Ribeiro AG, da Cruz LP, Marchi KC, Tirapelli CR, Miasso AI. Antidepressivos: uso, adesão e conhecimento entre estudantes de medicina. Ciênc Saude Coletiva. 2014;19(6):1825–33. doi: 10.1590/1413-81232014196.06332013.
Assem-Hilger E, Jungwirth S, Weissgram S, Kirchmeyr W, Fischer P, Barnas C. Benzodiazepine use in the elderly: An indicator for
inappropriately treated geriatric depression? Int J Geriatr Psychiatry. 2009;24(6):563–9. doi: 10.1002/gps.2155
Szwarcwald CL, Stopa SR, Damacena GN, Almeida WS, Souza Júnior PRB, Vieira MLFP, et al. Changes in the pattern of health services use in brazil between 2013 and 2019bl health journal. Ciênc Saude Coletiva. 2021;26(suppl1):2515–28. doi: 10.1590/1413-81232021266.1.43482020.
Berrouet Mejía MC, Lince Restrepo M, Restrepo Bernal D. Actitudes, conocimientos y prácticas frente a la automedicación con productos herbales y psicofármacos en estudiantes de medicina de Medellín-Colombia. Med UPB. 2018;37(1):17–24. doi: 10.18566/medupb.v37n1.a03.
Telles Filho PCP, Pereira Júnior AC. Antidepressivos: Consumo, Orientação E Conhecimento Entre Acadêmicos De Enfermagem. Rev Enferm Cent O Min. 2013;3(3):829–36. doi: 10.19175/recom.v0i0.411.
Martins de Oliveira L, Pereira de Menezes Filho AC, Porfiro CA. Uso da Passiflora incarnata L. no tratamento alternativo do transtorno de ansiedade generalizada. Res Soc Dev. 2020;9(11):e2349119487. doi: 10.33448/rsd-v9i11.9487.
Abi-Ackel MM, Lima-Costa MF, Castro-Costa E, Loyola Filho AI. Uso de psicofármacos entre idosos residentes em comunidade: prevalência e fatores associados. Rev Bras Epidemiol. 2017;20(1):57–69. doi: 10.1590/1980-5497201700010005.
Deus MD, Schmitz MES, Vieira ML. Família, gênero e jornada de trabalho: uma revisão sistemática de literatura. Gerais, Rev Interinst Psicol. 2021;14(1):1–28. doi: 10.36298/gerais202114e15805.
Campo-Arias A, Suárez-Colorado YP, Caballero-Domínguez CC. Asociación entre el consumo de Cannabis y el riesgo de suicidio en adolescentes escolarizados de Santa Marta, Colombia. Biomed. 2020;40(3):569–77. doi: 10.7705/biomedica.4988.
Rotenstein LS, Ramos MA, Torre M, Bradley Segal J, Peluso MJ, Guille C, et al. Prevalence of depression, depressive symptoms, and suicidal ideation among medical students a systematic review and meta-analysis. JAMA. 2016;316(21):2214–36. doi: 10.1001/jama.2016.17324.
Candido FJ, Souza R, Stumpf MA, Fernandes LG, Veiga R, Santin M, et al. The use of drugs and medical students: A literature review. Rev Assoc Med Bras. 2018;64(5):462–8. doi: 10.1590/1806-9282.64.05.462.
Rabiee R, Lundin A, Agardh E, Hensing G, Allebeck P, Danielsson AK. Cannabis use and the risk of anxiety and depression in women: A comparison of three Swedish cohorts. Drug Alcohol Depend. 2020;216:108332. doi: 10.1016/j.drugalcdep.2020.108332.
Tovani JBE, Santi LJ, Trindade EV. Use of psychotropic drugs by students from the health area: a comparative and qualitative analysis. Rev Bras Educ Med. 2021;45(3):1–10. doi: 10.1590/1981-5271v45.3-20200485.ING.
Wang K, Liu Y, Ouedraogo Y, Wang N, Xie X, Xu C, et al. Principal component analysis of early alcohol, drug and tobacco use with major depressive disorder in US adults. J Psychiatr Res. 2018;100:113–20. doi: 10.1016/j.jpsychires.2018.02.022.
Amin-Esmaeili M, Rahimi-Movaghar A, Sharifi V, Hajebi A, Radgoodarzi R, Mojtabai R, et al. Epidemiology of illicit drug use disorders in Iran: prevalence, correlates, comorbidity and service utilization results from the Iranian Mental Health Survey. Addiction. 2016;111(10):1836–47. doi: 10.1111/add.13453.
Raposo JCDS, Costa ACQ, Valença PAM, Zarzar PM, Diniz AS, Colares V, et al. Binge drinking and illicit drug use among adolescent students. Rev Saude Publica. 2017;51:83. doi: 10.11606/S1518-8787.2017051006863.
Bhatti AB, Haq AU. The pathophysiology of perceived social isolation: effects on health and mortality. Cureus. 2017;9(1):e994. doi:
7759/cureus.994.
Gémes K, Forsell Y, Janszky I, László KD, Lundin A, Ponce De Leon A, et al. Moderate alcohol consumption and depression – a longitudinal population-based study in Sweden. Acta Psychiatr Scand. 2019;139(6):526–35. doi: 10.1111/acps.13034.
Wium-Andersen MK, Ørsted DD, Tolstrup JS, Nordestgaard BG. Increased alcohol consumption as a cause of alcoholism, without similar evidence for depression: a Mendelian randomization study. Int J Epidemiol. 2015;44(2):526–39. doi: 10.1093/ije/dyu220.
Blumenberg C, Barros AJD. Response rate differences between web and alternative data collection methods for public health research: a systematic review of the literature. Int J Public Health. 2018;63(6):765–73. doi: 10.1007/s00038-018-1108-4.
Bispo Júnior JP. Social desirability bias in qualitative health research. Rev Saude Publica. 2022;56:101. doi: 10.11606/s1518-8787.2022056004164.
Descargas
Publicado
Número
Sección
Licencia
Derechos de autor 2024 Telma Regina Fares Gianjacomo, Camilo Molino Guidoni, Renne Rodrigues, Selma Maffei de Andrade, Jéssica Vertuan Rufino, Edmarlon Girotto

Esta obra está bajo una licencia internacional Creative Commons Atribución 4.0.